Claims Status
The claim status inquiry functionality in the Provider Online Service Center allows you to verify the status of a claim submitted to MassHealth. After MassHealth processes a claim, the claim is given a 13-digit Internal Control Number (ICN). Providers can upload a 276 batch file and download the 277 response (HIPAA transaction sets) for the status of the claim through the Provider Online Service Center or through direct data entry (DDE) claims status panels.
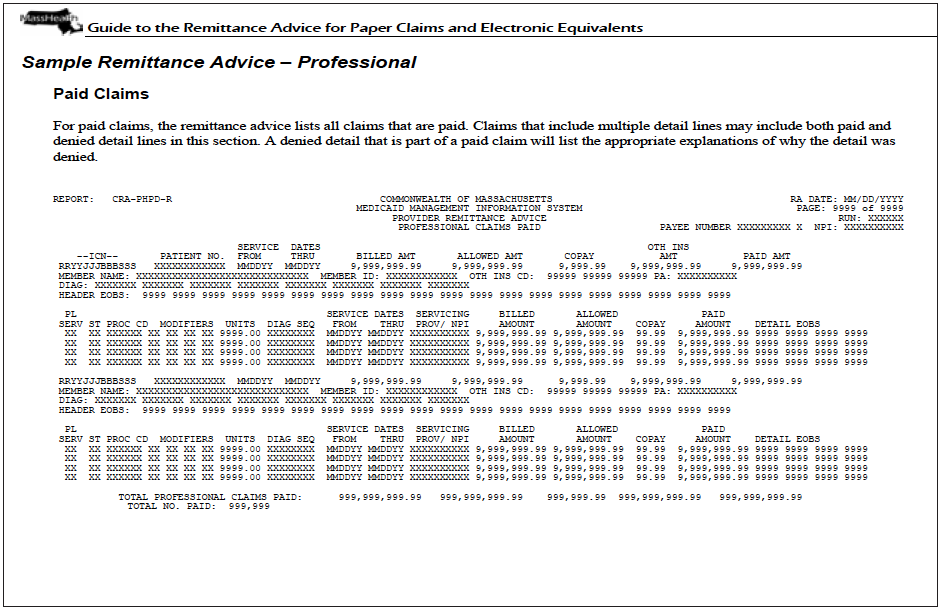
The status is also available on the MassHealth issued remittance advice (RA).
Claim Denials and Suspensions
Denials
Claims (both batch and DDE) that deny contain edit code(s) that describe the denial reason. These claims must be reviewed, corrected (if applicable), and resubmitted to MassHealth within the appropriate time frame. To visit the list of edits that can appear on the RA, please see the List of Explanation of Benefit Codes appearing on the Remittance Advice and other additional aids listed in the Additional Claims Resources section below.
Suspensions
A suspended claim is a claim that requires review before final adjudication. When a claim appears as suspended on a remittance advice (RA), the ICN assigned to the claim will remain the same throughout the processing cycle. You should post the claim as received by MassHealth. Do not rebill the claim while it is in suspense. The suspended claim will appear on a subsequent RA as paid or denied.
Remittance Advice (Claim Status Reporting)
A Remittance Advice (RA) is a report that provides claims processing status to providers indicating if the claim is paid, denied, or suspended (please see additional information below regarding denied and suspended claims). The RA is a helpful tool when reconciling accounts, as it reports the status of a claim submitted to MassHealth.
The RA is available in two forms: the 835 electronic RA, and the downloadable PDF RA, which is available online. The 835 (HIPAA transaction) RA can be downloaded from the POSC by a provider who has a signed Trading Partner Agreement (TPA) on file with MassHealth. The RA in PDF format also displays information about claim status, although it appears in a format that is unique to MassHealth. Providers can review, download, or print the PDF RA on the Provider Online Service Center.
Each Tuesday, the applicable RA is given a 6-digit run number, e.g., 100139, one week and 100140 the next week. On a weekly basis, the Remittance Advice is posted on POSC for providers.
MassHealth Provider Remittance Advice Message Text webpage
MassHealth has a historical listing of message texts that have appeared on provider Remittance Advices available on Mass.gov
Additional Claims Resources
Many claims are denied due to eligibility. For more information about checking member eligibility, please go to the following web pages.
Eligibility Verification System Overview Check Member Eligibility
MassHealth Billing and Claims, containing important information about billing and submitting claims
POSC job aids, including denied claims correction and adjustments
Billing Tips is an assortment of informational leaflets that summarize policies and procedures, including using RA to reconcile accounts
List of Explanation of Benefit Codes Appearing on the Remittance Advice
Information regarding 835, including Claim Adjustment Reason Codes (CARC) and Remittance Advice Remark Codes (RARC)
Timely Filing Bulletins—
- All Provider Bulletin 233: Revisions to the 90-Day Waiver Procedures
- All Provider Bulletin 232: Revisions to the Final Deadline Appeal Procedures
- All Provider Bulletin 300: Final Deadline Appeals Board Electronic Correspondence
Learn more about Adjusting/replacing a paid claim.

| Date published: | July 29, 2022 |
|---|