Introduction
Coinciding with the rise of the opioid crisis, there has been a sharp increase in the incidence of neonatal abstinence syndrome (NAS) among infants born in the United States since 2010, a trend seen even more acutely in Massachusetts. [1] NAS is a condition that can affect a subset of infants with prenatal exposure to opioids as a result of the mother’s use of opioids and/or prescribed medication for addiction treatment (MAT). The diagnosis is characterized by a constellation of symptoms that typically develop in the first few days after birth, and can include fever, difficulty feeding, and sleep disturbances, or include more severe symptoms such as excessive weight loss and seizures. Despite the risk for an infant developing NAS, treatment for opioid-use disorder (OUD) with MAT during pregnancy is medically recommended by clinical experts and has been associated with improved maternal and fetal outcomes when compared to pregnancies involving untreated OUD. [2,3,4,5]
Caring for infants with NAS can be complex and costly. In 2012, the national average inpatient stay after birth for infants diagnosed with NAS was 16.9 days, with a mean hospital charge per stay of $66,700. In comparison, the mean hospital charge for an uncomplicated term infant birth was $3,500. [6] Traditionally, infants diagnosed with NAS have required care in a neonatal intensive care unit (NICU) or special care nursery for administration of pharmacotherapy and observation of symptoms. While pharmacotherapy may be necessary to relieve symptoms, it can increase length of stay, contribute to overtreatment, and increase costs. Locating infants in a higher-acuity setting can also interfere with the mother-infant bonding process and may contribute to the stigma mothers with OUD face in health care settings. [7] Emerging evidence suggests a family-centered approach in a lower-acuity setting involving substance use treatment for mothers and symptom prevention and management for infants may be preferable and more cost-effective. [8,9]
To address the rise of NAS in Massachusetts and improve health outcomes and reduce costs, the Massachusetts Health Policy Commission (HPC) launched its $3 million Mother and Infant-Focused Neonatal Abstinence Syndrome Interventions (NAS Interventions) in 2016. The HPC’s NAS Interventions aim to contribute to the Commonwealth’s nation-leading efforts to address the opioid crisis by supporting new evidence-based interventions and emerging best practices to treat mothers and infants impacted by OUD.
This issue of DataPoints provides an overview of the prevalence of NAS in Massachusetts and highlights improved outcomes associated with the NAS Interventions, which demonstrate significant promise as better, more cost-effective care. The interactive graphics below will display best in full screen mode. Scroll to the bottom of each graphic and click on the far-right icon to view them in full screen mode. Use the same icon to return to the original view.
Prevalence of Neonatal Abstinence Syndrome in Massachusetts
The number of substance-exposed newborns (SEN) and infants diagnosed with NAS in Massachusetts increased between 2010 and 2017, as shown in Figure 1 below. In 2017, 15.9 infants were diagnosed with NAS per 1,000 hospital births in Massachusetts, nearly double the most recently reported national rate of eight infants per 1,000 hospital births in 2014. [10] Figure 2 displays the rate of SEN and NAS births by region and by birthing hospital in Massachusetts, reflecting the variation in the impact of SEN and NAS across the Commonwealth.
HPC Awards: Supporting Innovative Models of Care
In 2016, the HPC launched the NAS Interventions to further test and accelerate the adoption of evidence-based interventions and emerging best practices to treat mothers and infants impacted by OUD. As part of the Health Care Innovation Investment (HCII) program, the HPC awarded nearly $3 million to six hospitals. [11] Awards ranged from $250,000 to $1 million for a performance period of 12 or 24 months. The participating hospitals were Baystate Medical Center, Boston Medical Center, Lahey Health - Beverly Hospital, Lawrence General Hospital, Lowell General Hospital, and UMass Memorial Medical Center. The Neonatal Quality Improvement Collaborative of Massachusetts (NeoQIC) provided technical assistance to the participating hospitals.
HPC NAS Care Models
Across all sites, the hospitals implemented various interventions to improve care and reduce length of stay for infants. Key components included:
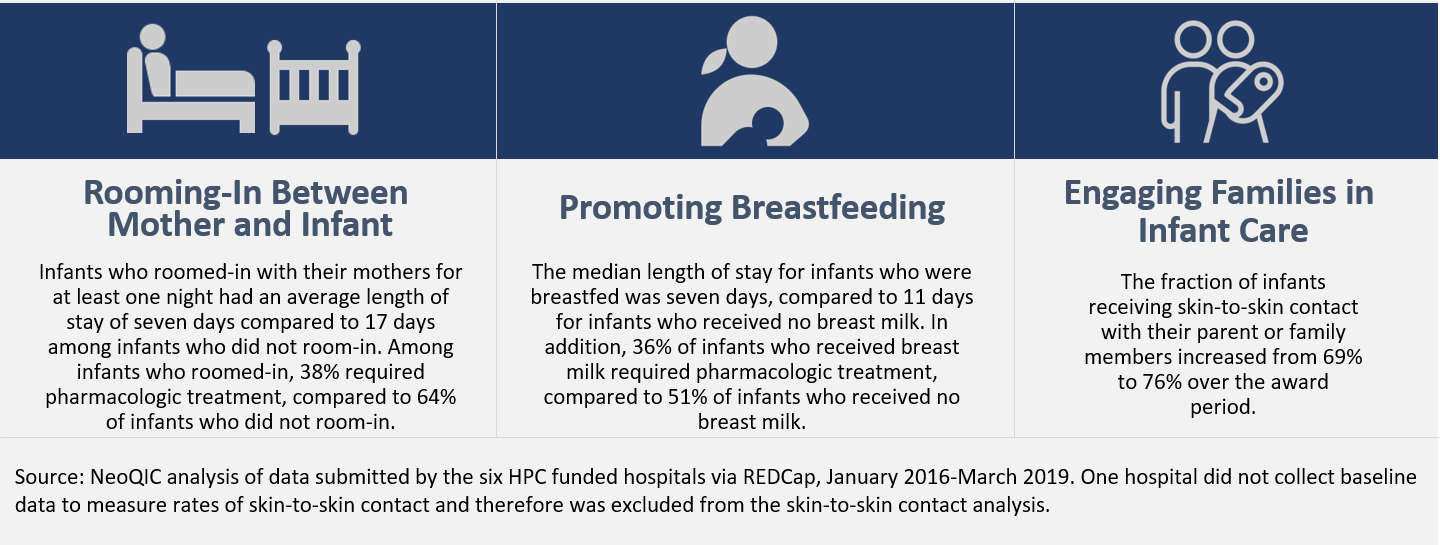
- Increasing non-pharmacologic interventions. Hospitals focused on promoting non-pharmacologic interventions such as rooming-in, skin-to-skin contact, breastfeeding, and sustained maternal presence at the infant’s bedside, particularly after maternal discharge. These approaches have been seen to reduce symptoms of NAS and the need for pharmacologic intervention, and encourage maternal involvement in the care of the newborn. See Figure 3 below for more information.
- Optimizing NAS pharmacologic treatment. Hospitals standardized assessment and scoring of NAS symptoms and optimized protocols for pharmacologic treatment. Some programs standardized their use of the Finnegan scoring system, while others implemented the Eat, Sleep, Console model.
- Increasing access to services for mother and infant after discharge. Hospitals implemented NAS discharge care plans, and eased transitions to family support, peer counseling, early intervention services, and primary care.
While all hospitals implemented these core components, they adapted their care models to their particular practice settings and population needs. Hover over the icons in the figure below to learn more about each care intervention.
Program Outcomes
The quality improvement efforts implemented by the awardee hospitals were associated with multiple positive outcomes among term infants (i.e., infants born at >37 weeks) at risk for NAS. Compared to baseline data, hospitals observed a 53% reduction in median hospital length of stay for infants, decreasing from 17 days to 8 days over the 24 months following program launch. Much of this reduction is attributed to the reduced need for pharmacologic therapy, which decreased 36%, from 66% of infants to 42% of infants. Because pharmacologic therapy is often administered in the NICU or special care nursery, hospitals also observed a 23% decrease in the percentage of infants requiring care in the NICU or special care nursery. Shorter stays and less reliance on the NICU or special care nursery have significant implications for cost savings. The figures below highlight some of the promising outcomes observed during the performance period.
The promotion of non-pharmacologic interventions was a critical driver of these positive changes. Hospitals found that non-pharmacologic interventions are an effective treatment for NAS symptoms used in parallel to pharmacologic treatment or, when appropriate, as an alternative to pharmacologic treatment. Furthermore, these practices also promote maternal-infant bonding and center the mother and family in treatment, contributing to positive long-term family outcomes.
Conclusion
As Massachusetts continues to grapple with the effects of the opioid epidemic, mothers and infants affected by opioid use and NAS may benefit from new, evidence-based care models. As highlighted in this DataPoints issue, care models that promote the use of non-pharmacologic interventions and emphasize mother-infant bonding have been associated with a reduction in infant length-of-stay and offer a promising opportunity to improve care for mothers and infants impacted by opioid use disorder. With the support of the Department of Public Health and in partnership with NeoQIC, the HPC continues to support the adoption of these interventions across the Commonwealth. Visit our website for more information about the HPC’s NAS Interventions and to see hospital program profiles.
Sources: HPC Opioid-Related Acute Hospital Utilization Chart Pack 2019; NeoQIC analysis of data submitted by the six HPC funded hospitals via REDCap, January 2016-March 2019.
Additional Resources
Notes
[1] Massachusetts Health Policy Commission. Opioid-Related Acute Hospitalization Utilization. June 2019.
[2] American College of Obstetricians and Gynecologists. Medication-Assisted Treatment Remains the Recommended Therapy for Pregnant Women. July 2017.
[3] Jones, H. E., O’ Grady, K. E., Malfi, D. Tuten, M. Methadone maintenance versus methadone taper during pregnancy: maternal and neonatal outcomes. Am. J. Addict. 17, 372–386 (2008).
[4] Connaughton, J. F., Reeser, D., Schut, J. Finnegan, L. P. Perinatal addiction: outcome and management. Am. J. Obstet. Gynecol. 129, 679–686(1977).
[5] Kaltenbach, K., Berghella, V. Finnegan, L. Opioid dependence during pregnancy. Effects and management. Obstet. Gynecol. Clin. North Am. 25, 139–151 (1998).
[6] Patrick SW, et al. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinatol. 2015;35:650–655.
[7] Newman A, Davies GA, Dow K, et al. Rooming-in care for infants of opioid-dependent mothers: Implementation and evaluation at a tertiary care hospital. Can Fam Physician. 2015;61(12):e555–e561.
[8] American College of Obstetrics and Gynecologists. Opioid Use and Opioid Use Disorder in Pregnancy. August 2017.
[9] Substance Abuse and Mental Health Services Administration. Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants. HHS Publication No. (SMA) 18-5054. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2018.
[10] Winkelman, T. N., Villapiano, N., Kozhimannil, K. B., Davis, M. M., & Patrick, S. W. (2018). Incidence and Costs of Neonatal Abstinence Syndrome Among Infants With Medicaid: 2004–2014. Pediatrics, 141(4). doi:10.1542/peds.2017-3520
[11] Combined funding from the HPC and the “Moms Do Care” program, as administered by the Massachusetts Department of Public health and funded by SAHMSA.
Contact for HPC DataPoints, Issue 15: Mother and Infant-Focused Neonatal Abstinence Syndrome Investments
Online
Phone
HPC-Info@state.ma.us
Address
| Date published: | September 26, 2019 |
|---|