Office of Long Term Services and Supports (OLTSS)
Programs and services managed by the Office of Long Term Services and Supports (OLTSS) enable hundreds of thousands of people with disabilities
and chronic conditions in Massachusetts to:
- live with independence and dignity in their daily lives;
- participate in their communities to the fullest extent possible; and
- improve their overall quality of life.
Most people receive these services in their home or at community programs. Some people get these services in a facility where they live, such as a nursing facility. Provider types managed by OLTSS and links to the provider manuals for each:
- Adult Day Health
- Adult Foster Care
- Chronic Disease and Rehabilitation (CDR) Inpatient Hospital
- Chronic Disease and Rehabilitation (COH) Outpatient Hospital
- Continuous Skilled Nursing (CSN) Agency
- Day Habilitation
- Durable Medical Equipment (DME) Competitive Bid
- Durable Medical Equipment (this includes a pharmacy that provides DME)
- Fiscal Intermediary (Personal Care)
- Group Adult Foster Care
- Group Practice Therapists (PT/OT/ST)
- Home Health Agency
- Hospice
- Independent Nurse
- Independent Living Centers (Personal Care)
- Individual Therapists (PT/OT/ST)
- Nursing Facilities
- Orthotics
- Oxygen and Respiratory Therapy Equipment
- Personal Care Attendant
- Prosthetics
- Rehabilitation Centers
- Speech and Hearing Centers
Office of Behavioral Health — Fee-for-Service
MassHealth’s behavioral health program offers its members a diverse set of resources to manage their behavioral health needs. There are a variety of behavioral health services (mental health and substance use disorder) to address each member’s individual need. Behavioral health services range from acute psychiatric inpatient care to outpatient counseling services, such as individual, group, couple or family therapy, and substance use disorder treatment. Psychological and neuropsychological assessments are also available.
Behavioral health services are offered in a variety of settings, such as an inpatient or outpatient hospital, mental health or substance use disorder outpatient clinic, member’s home, private office, and/or nursing facilities.
Provider types managed by the Office of Behavioral Health:
Dental — Fee-for-Service
The mission of the MassHealth Dental Program is to expand access to high-quality and compassionate oral health services. Dental care is one of many benefits available to children and adults who are eligible for MassHealth, the Health Safety Net, and the Children’s Medical Security Plan. The MassHealth dental program regulations at 130 CMR 420.000 and 450.105 describe the dental benefit, service limitations, and member eligibility.
There are two categories of care under MassHealth’s Dental Benefit:
- Dental services utilizing ADA/CDT codes which are submitted to the dental portal hosted by DentaQuest, where all prior authorization (PA) requests and claims adjudications are processed.
- Medical Services/Oral Surgery utilizing CPT/ HCPCS codes which are submitted to the Mass- Health Provider Online Service Center (POSC/ Portal)
MassHealth has contracted with Dental Service of Massachusetts, Inc. (DSM) to manage the MassHealth dental program. DSM and its subcontractor, DentaQuest, LLC (DentaQuest) work with MassHealth to help improve the MassHealth dental program. Dental services covered by MassHealth are:
- Exams and radiographs
- Teeth cleaning and fluoride treatment
- Tooth fillings
- Crowns for children younger than 21
- Partial and complete dentures
- Tooth extraction
- Oral surgery
Dental providers must complete an application to enroll with MassHealth to bill for dental services utilizing App Central at App Central. Additionally, dental providers must create an account on the MassHealth dental provider web portal to check member eligibility, service history, submit claims and perform other essential administrative tasks.
For assistance, please contact DentaQuest customer service at (800) 207-5019 between the hours of 8 a.m. to 6 p.m., Monday through Friday.
To view MassHealth covered dental services, please see Subchapter 6 Dental Service Codes of the Dental Manual.
Oral Surgeons
Oral surgeons who are enrolled as a MassHealth dental provider must also enroll to bill oral surgery CPT/medical codes via MassHealth’s Provider Online Service Center (POSC) by filling out a Data Collection Form.
For Oral surgery CPT medical Covered Services please see Subchapter 6 Dental Service Codes of the Dental Manual.
***SPECIAL NOTICE***
All Integrated Care Organization (ICO), Senior Care Organization (SCO), and Program of All-Inclusive Care for the Elderly (PACE) plans listed below may have a different dental policy than MassHealth.
Please review the dental policy for each plan.
- BMCHP
- Common Care Alliance
- Fallon/Navicare
- Senior Whole Health
- Tufts Health Unify
- United Health Care
- One Care
Pharmacy — Fee-for-Service
The MassHealth Pharmacy Program provides pharmacy coverage for more than one million members of the Commonwealth for acute and chronic prescription medications as well as certain over-the-counter products and professional services such as vaccines. The program manages a robust formulary known as the MassHealth Drug List (MHDL) for its members while maintaining clinical appropriateness and cost savings. Included in the MHDL are initiatives that the pharmacy program has put in place to better serve the member’s course of therapy, such as the Pediatric Behavioral Health Initiative (PBHMI) and the Concomitant Opioid Benzodiazepine Initiative (COBI). The Pharmacy Program uses the Pharmacy Online Processing System (POPS) for claim submission for Mass- Health ACOB and Fee-for-Service plans as well as the Health Safety Net (HSN) and Children’s Medical Security Plan (CMSP). Providers can find information about POPS, including helpful billing tips, in the POPS Billing Guide.
More information on the MassHealth Pharmacy Program, including links to the MassHealth Drug List, Pharmacy Regulations, Pharmacy Facts, Publications and Notices can be found at MassHealth Pharmacy Program
MassHealth Pharmacy Regulations: 130 CMR 406.000: Pharmacy Services
MassHealth Pharmacy Facts: MassHealth Pharmacy Facts
MassHealth Drug List: MassHealth Drug List - Health and Human Services
Specialists and Hospitals — Fee-for-Service
The MassHealth Fee-for-service program within the Office of Provider and Pharmacy Programs includes ambulatory services that are paid per service rendered. These services are rendered by the following providers:
- Acute Inpatient Hospitals
- Acute Outpatient Hospitals and Hospital Licensed Health Centers (HLHCs)
- Acupuncture Services
- Audiologists
- Community Health Centers
- Family Planning Agencies
- Freestanding Abortion and Sterilization Clinics
- Freestanding Ambulatory Surgery Centers (FASCs)
- Freestanding Renal Dialysis Clinics
- Hearing Instrument Specialists
- Independent Clinical Laboratories
- Independent Diagnostic Testing Facilities (IDTFs)
- Optometrists
- Opticians
- Podiatrists
- Chiropractor
- Physicians
- Nurse Practitioners
- Nurse Midwives
- Physician Assistants
- Certified Nurse Specialists
- Psychiatric Certified Nurse Specialists
- Certified Registered Nurse Anesthetist
- Urgent Care Clinics
Acute Outpatient Hospital Program
MassHealth pays for outpatient hospital visits and ancillary services (such as radiographic views, laboratory tests, medical supplies, and drugs) that are medically necessary and appropriately provided, as defined at 130 CMR 450.204: Medical Necessity. The quality of such services must meet professionally recognized standards of care.
As defined in 130 CMR 410.000: Outpatient Hospital Services, “hospital outpatient department” may also refer to hospital-licensed health centers and other hospital satellite clinics.
Acute Inpatient Hospital Program
MassHealth pays for inpatient hospital services that are medically necessary and appropriately provided as defined by 130 CMR 450.204: Medical Necessity. The quality of such services must meet professionally recognized standards of care.
As defined in 130 CMR 415.000: Acute Inpatient Hospital Services, “hospital” refers specifically to an acute inpatient hospital or unit only, unless the context clearly indicates otherwise.
For more information about acute hospital programs, including eligibility, regulations and specific information for patients and providers, visit the following web pages:
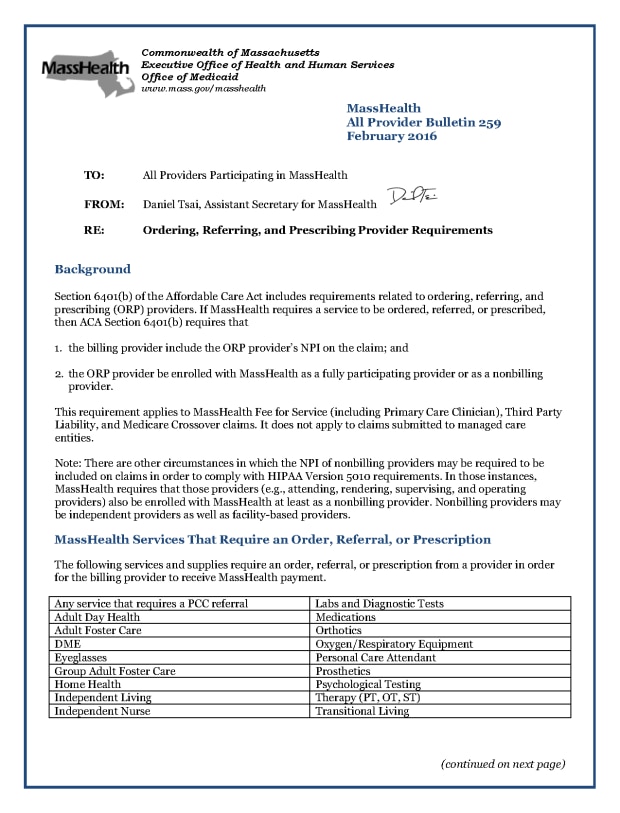
Ordering, Referring, and Prescribing (ORP)
Section 6401(b) of the Affordable Care Act (ACA) includes requirements related to ordering, referring, and prescribing (ORP) providers. If MassHealth requires a service to be ordered, referred, or prescribed, then ACA Section 6401(b) requires that the billing provider include the ORP provider’s national provider identifier (NPI) on the claim and the ORP provider must be enrolled with MassHealth in order for the claim to be payable. An ORP provider can be enrolled with MassHealth as a fully participating provider or as a non-billing provider. For the claim to be payable, only certain types of providers may be listed on a claim as the ordering, referring, or prescribing provider, referred to as authorized ORP providers. For more information about ORP requirements, including the services that require ORP and provider types authorized to Order, Refer, or Prescribe, please refer to the following provider bulletins:
You can also learn more on the ACA ORP Requirement for MassHealth Providers web page.
Qualified Medicare Beneficiaries (QMB) Provider
A Qualified Medicare Beneficiaries (QMB)-only provider is a provider who provides medical services only to MassHealth Senior Buy-In members described in 130 CMR 519.010: MassHealth Senior Buy-In and in 130 CMR 505.007: MassHealth Senior Buy-In and Buy-In and certain MassHealth Standard members who are eligible for QMB benefits described in 130 CMR 519.002(A)(4)(c) and 130 CMR 505.002(O). QMB-only providers are subject to all regulations pertaining to providers participating in MassHealth, except as provided below or as otherwise specified in 130 CMR 450.000: Administrative and Billing Regulations. QMB-only providers may bill only for medical services for QMB members and Standard members eligible for QMB benefits, whether or not the associated medical services are specified in 130 CMR 400.000 through 499.000.
Health Safety Net (HSN)
Health Safety Net (HSN) pays only acute care hospitals and community health centers for certain essential health care services provided to qualified uninsured and underinsured Massachusetts residents. HSN is available to uninsured and underinsured Massachusetts residents whose family income is less than a certain percentage of the Federal Poverty Level (FPL). Learn more about HSN, including eligibility, regulations, and specific information for patients and providers, on the Health Safety Net web page.
HSN Dental Providers
The Health Safety Net pays for the same set of dental services that are covered by MassHealth Standard, plus certain services currently not covered by MassHealth.
Patients may be determined eligible only for the HSN or may be determined eligible for MassHealth with HSN as a secondary payer for certain services. The Health Safety Net prices dental services using MassHealth’s dental fee schedule.
As of January 1, 2017, DentaQuest administers the Health Safety Net Dental program. HSN dental providers submit dental claims directly to DentaQuest for processing and pricing. The Health Safety Net makes a monthly payment to providers, which includes payment for both medical and dental services. This Office Reference Manual provides important information for HSN providers about eligible dental services, claims, clinical criteria, and other processes.
DentaQuest Customer Service
For assistance, please contact DentaQuest customer service at (800) 207–5019 between 8 a.m. and 6 p.m., Monday through Friday.
Additionally, you can reach DentaQuest through the MassHealth Dental Program home page and the MassHealth/HSN Dental Provider Web Portal.
Children’s Medical Security Plan (CMSP)
The Children’s Medical Security Plan (CMSP) provides primary and preventive medical, behavioral health, and dental coverage to uninsured children younger than 19 years of age who do not qualify for any MassHealth coverage types (other than MassHealth Limited). CMSP program regulations are found at 130 CMR 522.004.
For more information about CMSP, please visit the Children’s Medical Security Plan web page for current eligible providers and services, covered codes, and prior authorizations.
Community Partners
The MassHealth Community Partners Program coordinates person-centered, community-based supports that promote continuity of care and independence for MassHealth members with behavioral health (BH) or long-term services and supports (LTSS) needs. While the majority of eligible members are identified by ACOs/MCOs or MassHealth, healthcare providers may also refer a member to the Community Partners Program by contacting the member’s health plan (i.e., ACO or MCO).
Across the Commonwealth, BH and LTSS Community Partners bring together community resources, health plans and primary care providers (PCPs) to ensure that eligible members receive the right scope and intensity of care in the community. Community Partners can help coordinate services and supports such as health and wellness coaching, assistive hearing and vision devices, durable medical equipment, medication reconciliation, personal care assistance, and home health aide services. Community Partners can also help connect members with behavioral health services, day programs (such as adult day health and adult foster care), and other programs such as food stamps, fuel assistance, and Meals on Wheels. Community Partners can also help the pediatric population access community-based services and supports.
Learn more about the Community Partners Program.
| Date published: | July 29, 2022 |
|---|