About
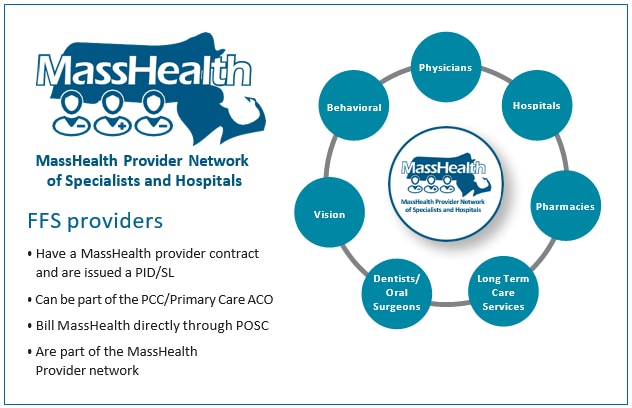
MassHealth offers benefits on a Fee-for-Service (FFS) basis or through managed care plans.* Under the FFS model, MassHealth pays providers directly for each covered service received by an eligible MassHealth member. MassHealth also pays network providers directly for services provided to Primary Care Clinician (PCC) Plan and Primary Care Accountable Care Organization (ACO) members. Providers would bill MassHealth directly for services provided to such members. Each provider in the FFS network is issued a Provider Identification/ Service Location number (PID/SL). These providers use the Provider Online Service Center (POSC) to submit claims into MassHealth’s Medicaid Management Information System (MMIS) system in addition to other functions described in this handbook.
MassHealth Network providers are enrolled in MassHealth as contracted providers via a provider agreement and are required to furnish medical services and participate in MassHealth under a provider contract with the MassHealth agency. For purposes of applying, in regulations 130 CMR 450.235 through 450.240, the term “provider” includes formerly participating providers.
*Please note that other Managed Care Plans such as Managed Care Organizations (MCO), Senior Care Options (SCO), Program of All-inclusive Care for the Elderly (PACE), One Care, and Accountable Care Partnership Plans (ACPP) have separate provider networks and contracts. Providers must have contracts with these plans to service their members and receive payment for services rendered.
| Date published: | July 29, 2022 |
|---|