Read the Report
Click here to read the 2022 Health Care Cost Trends Report.
About this Report
The Attorney General’s Office examines how a commonly-used calculation for determining health care payments fails to accurately measure health needs and causes funding to be moved away from low-income communities in Massachusetts. Confidential insurance company data and public data from the Massachusetts Department of Public Health is used to examine four topics:
- How population health risk scores compare with community-level indicators of health and health care access.
- How the Centers for Medicare & Medicaid Services (CMS) risk adjustment program shifts funds across insurers serving different populations
- How changes to the CMS risk adjustment formula could address the unintended consequences of these transfers.
- How service closures and lack of capital investment by hospitals in low-cost networks risk further limiting access to care in the same low-income communities where utilization is already lower than social determinants of health would predict.
Health Scores and Access Barriers
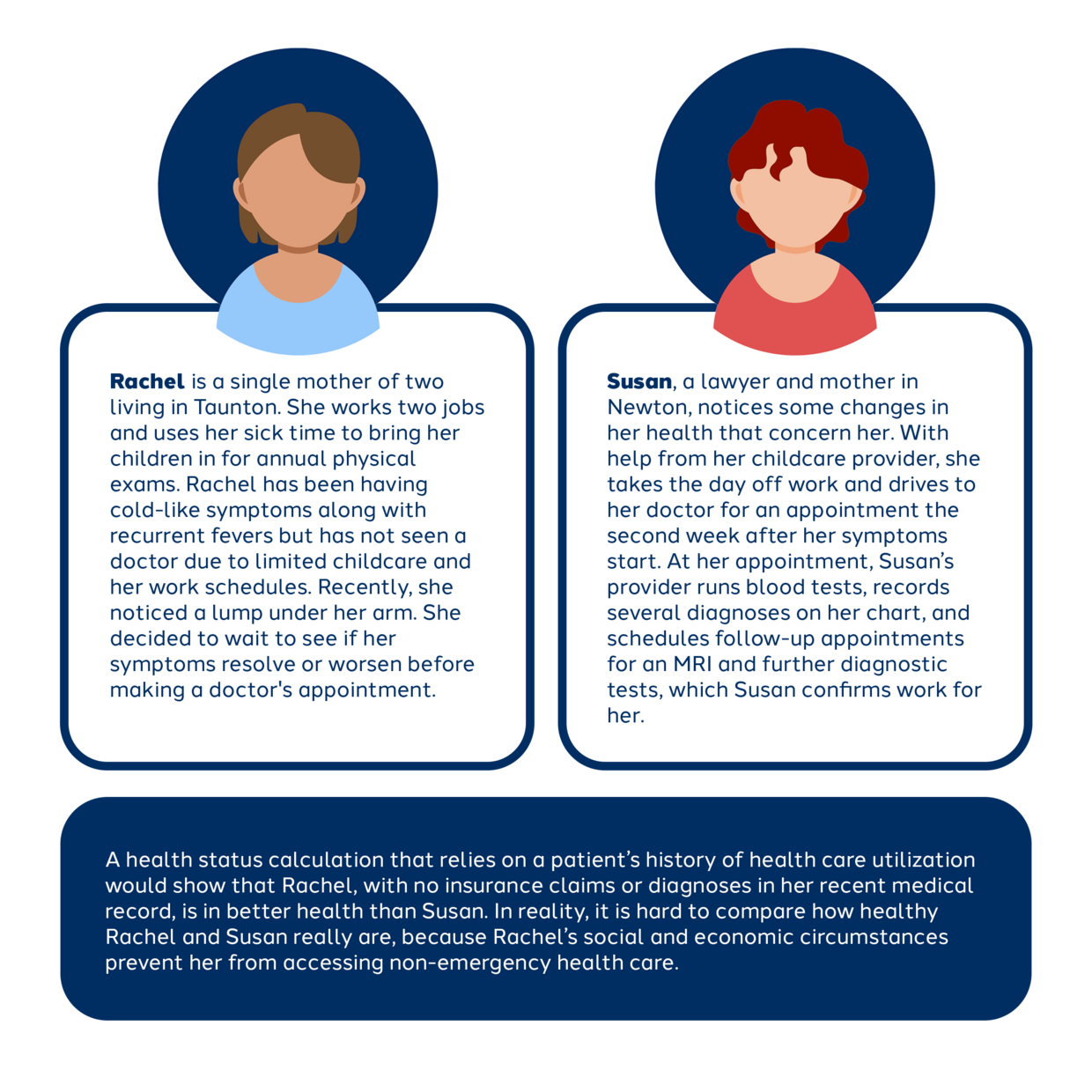
Health risk scores based upon a population’s history of health care utilization entrench resource disparities and health care access barriers. Communities who face barriers that depress their use of health care – like difficulties accessing transportation, housing, childcare, or broadband – are coded as “healthier,” contributing to a cycle of underfunding for their health care services. In the Massachusetts merged market (where individuals and small businesses buy insurance coverage), insurers that serve populations coded by CMS as “lower risk” actually serve communities with higher neighborhood stress scores, worse self-reported health scores, more barriers to accessing health care services, and lower rates of preventive care.
Risk Adjustment Transfers
The CMS risk adjustment program in the Massachusetts merged market shifts resources away from safety net providers and lower-income communities. Since the program’s implementation in 2014, these transfers have shifted hundreds of millions of dollars from insurers serving lower-income communities to insurers serving higher-income communities.
The transfer of funds away from insurers with low-priced provider networks is amplified because the formula for calculating transfers owed across insurers uses the statewide average premium, rather than a lower multiplier. This feature of the formula means that lower-cost insurers subsidize the higher prices of the providers in higher-cost insurer networks.
Hospital Service Closures and Capital Investment
The risk adjustment program’s redistribution of dollars away from insurers that contract with low-cost hospitals correlates with — and may compound — access challenges that low-income communities face because of essential health service closures and lack of capital investment by hospitals that serve those communities. Using DPH data, the Attorney General’s Office finds that hospitals in lower-cost insurer networks are both (a) more likely to close services deemed by DPH to be necessary for preserving access and health status and (b) less likely to make significant capital investments in their own facilities.
Conclusion and Recommendations
The inequitable distribution of health care resources — that is, the distribution of health care dollars in ways that do not align with health need and health burden — is itself a driver of aggregate health care cost increases. Risk adjustment, and other programs designed to redistribute health care resources to align with needs, presents an opportunity to rectify this inequity by incorporating data on a patient and community’s social determinants of health when estimating health needs.
Based on these findings, the Attorney General’s Office recommends:
- Payers and providers should incorporate social determinants of health, such as access to transportation, housing, childcare, and broadband, into approaches to health status adjustment, as MassHealth has done in its Accountable Care Organization program.
- Payers and providers that benefit from these new approaches suggested in the first recommendation should use the additional resources they receive to implement new initiatives or expand existing initiatives to help patients facing social and economic barriers to accessing health care services overcome these barriers.
- Massachusetts state agencies should partner with CMS to scrutinize equity implications of the CMS risk adjustment methodology, including by examining opportunities to include social determinants of health and modify the use of the statewide average premium.
- Massachusetts policymakers should pursue fundamental changes to health care cost containment policy with the goal of preserving safety net providers, such as flexible commercial price growth benchmarks that allow lower-priced providers more room for price growth than higher-priced providers.
These findings demonstrate the importance of health equity considerations in how government agencies and health care market participants measure population health, and how they use that information to distribute health care resources. Health status adjustment formulas should be scrutinized to ensure that tools used to assess the health needs of different groups do not perpetuate longstanding resource disparities.