ACO Composition and Governance Structure
Merrimack Valley Accountable Care Organization (MVACO) is a formalized partnership between Greater Lawrence Family Health Center (GLFHC) and Lawrence General Hospital (LGH) representing 130 primary care providers across 16 practices, formed to improve the care of Medicaid patients in the greater Lawrence community. Although this is a new organization, LGH and GLFHC have a shared history of working together for the benefit of the community, providing a strong model for primary care with GLFHC a federally qualified health center, designated an NCQA Level III PCMH and sharing a family practice residency program with LGH to help ensure the future of primary care resources in the community.
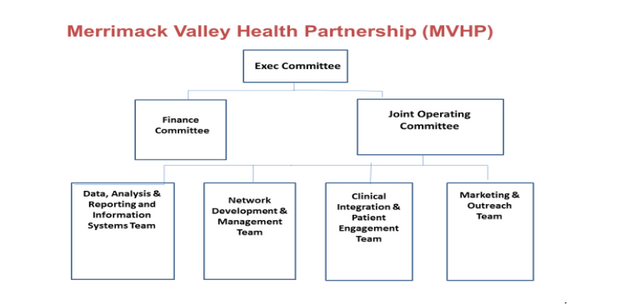
MVACO and Neighborhood Health Plan (NHP) formed the Accountable Care Partnership Plan named Merrimack Valley Health Partnership (MVHP). Merrimack Valley Health Partnership’s member facing name is My Care Family. Neighborhood Health Plan also has a long history of providing health insurance coverage as a Medicaid MCO for more than 10,000 patients treated by the GLFHC with experience in specialized care management and a strong relationship with Beacon Health Options for its behavioral health network and expertise. NHP, LGH and GLFHC have spent nearly a year developing an integrated organizational foundation for the ACO partnership plan contracted with EOHHS. Below is a high level organizational chart.
The participating entities come together via an Executive Committee, supported by the Finance and Joint Operating Committees (JOC). JOC recommendations are made to the Executive Committee, which has final approval for MVHP policy and strategic direction. The Executive Committee is comprised of the President of NHP and the Presidents of LGH and GLFHC, who are specifically authorized by their respective governing bodies to make binding decisions on behalf of their organizations concerning MVHP activities. The Executive Committee is supported by four (4) senior staff members from NHP and MVACO. The Executive Committee meets bimonthly and on an ad hoc basis as required. The following actions require approval of the Executive Committee; all investments of DSRIP Payments from EOHHS; annual plans submitted by the Joint Operating Committee including strategic, business, operations, marketing, care management and data integration plans; any material change to the prior authorization requirements; any material change to the composition of Network Providers; and annual operating budget, risk-sharing methodologies and settlements.
The Finance Committee reviews and makes recommendations to the Executive Committee with respect to the financial policies for MVHP, providing strategic guidance for the MVHP’s allocation of capital to its businesses, methods of financing its businesses, value based payment methodologies and other related strategic initiatives. Additionally, the Finance Committee oversees strategic and financial operational compliance with the EOHHS Contract, including but not limited to: (i) review and recommendations for the annual budget and advising on budget issues that arise during the budget process and throughout the year; (ii) Reviewing, on a regular basis, the MVHP’s financial performance relative to the budget.
The JOC, comprised of 9 operating team lead members, has overall responsibility to approve Care Management protocols and procedures; Care Needs Screenings to Enrollees; Comprehensive Assessments and documented Care Plans policies, Coordinating with BH CPs and LTSS CPs; developing, implementing and maintaining Wellness Initiatives and Disease Management Programs; and Developing, implementing and maintaining Transitional Care Management programs, including establishing appropriate protocols with Network hospitals, reviewing day to day activities of the MVHP and ensuring that both Parties are meeting their responsibilities under this Agreement, the Model Contract and the Provider Agreements. In addition, the JOC is responsible for preparing an annual strategic, business and operations plan, preparing reporting and data integration plans and processes; approving marketing plans and providing regular reports to the Executive Committee.
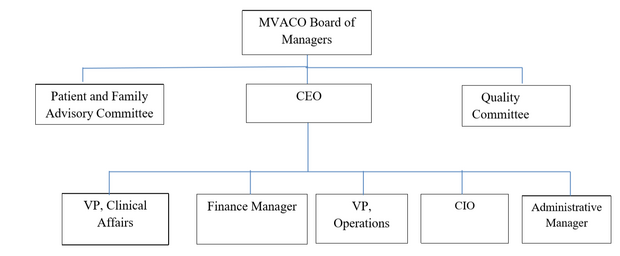
The organization chart below shows the local governance structure of the MVACO.
The MVACO is governed locally by a Board of Managers that is 75% controlled by providers or their designated representative, including representation from primary care, specialty care and mental health/substance abuse disorder treatment providers as well as a consumer/patient representative. The Board meets regularly to review, provide guidance and, as appropriate, vote on the following topics: Annual business plan, goals, and key performance metrics, Committee charters, goals, and metrics, functional integration with NHP, Annual operating and capital budgets, Financial reports, Gain / loss surplus or payment distribution models, Provider networks, Compliance and MVACO executive leadership.
The MVACO has achieved provisional ACO certification from the Health Policy Commission and will be working to achieve full certification for 2019. The provisional certification applies to new organizations with the understanding that many aspects are under development. For example, the Patient and Family Advisory Committee (PFAC) requirement is currently satisfied through using LGH’s PFAC structure that will be expanded to include ACO representation and topics during 2018. Additionally the quality committee is currently a combined group with NHP’s quality staff but will be refined during 2018 so that MVACO has a quality committee to lead local efforts for quality improvement and achieve the ACO quality goals.
ACO Population Served
According to the October, 2017 ACO PY1 DSRIP Funding notification letter, 33,907 members were attributed to MVACO for the service areas of Lowell, Lawrence and Haverhill. The overall service area population is approximately 276,263, focused primarily in Lawrence, Haverhill, Methuen and Lowell. Although the Hospital and Health Center’s service area population has an age distribution similar to that of the state; over 60% of the population is between the ages of 18 and 64, 20-30% are under the age of 18, and 8-14% are over the age of 65, the population has a low socio-economic status with health illiteracy contributing to the challenge of providing adequate health care to the population.
Lawrence is a diverse community, with 76% of the population Hispanic. Lawrence has one of the lowest median household incomes in the state ($34,000 versus $68,000 state average), as well as a high percent of families living below poverty (28%). The unemployment rate in the service area is higher than that of the state (9% versus 6%). Lawrence has 32% of residents without a high school diploma. Rents in the region are high and there is little quality affordable housing. In Lawrence, nearly half of renters (48%) contributed 35% or more of their household income towards housing.
These factors may contribute to a high disease burden and mortality rates, with Middleton, Lawrence and Methuen all above the state average. There is a higher than state average prevalence of diabetes in the service area, a higher rate of asthma related ED visits and greater rates of hospitalization for heart attack, coronary heart disease and stroke compared to the state. Also of concern is the teen birth rate and incidence of Chlamydia, Hepatitis B and C. The community lacks mental health care providers and reports long waitlists for services, which exacerbates conditions for those in need of critical care. Closely related to the issue of mental health in the community is the rising concern about substance use, particularly opiate use. Heroin use has nearly doubled across the service area communities in the past 5 years. Quantitatively, Lawrence and Haverhill have mental disorder hospitalization rates above the statewide rate.
GLFHC and LGH, along with multiple community partners, recently completed a population and community needs assessment that has been used to frame plans for addressing needs. Among the needs, adverse effects related to social determinants of health are pervasive for its patient population that is predominantly Latino, many of whom do not speak English, that is over 75% on Medicaid or without health insurance, that lacks sufficient food or shelter, and that has inadequate transportation and other resources to facilitate access to care. Only 65% of residents indicated they had at least one person or facility they considered their personal health care provider. For residents, the primary reason for not having one consistent health care provider was inability to communicate with providers (from a language perspective). These characteristics of the population provide many challenges including health illiteracy, where even if explained in their native language patients often do not understand their care plan and the need to take their medication, for example. Additionally, the patients sometimes travel to their home countries for months at a time making continuity of care very difficult. Even when here they move a lot or may not have a phone, so are hard to reach and stay in contact with. Despite these challenges, MVHP has designed a care model approach to be culturally competent and focused on connecting patients with primary care, behavioral health, LTSS and ongoing care management to better serve this complex patient population.
Overview of DSRIP Investment Approach
DSRIP decisions begin with a DSRIP planning committee that includes members of the 5 operating teams, with a focus on including provider leadership. A draft DSRIP plan is prepared by the planning committee and reviewed by the Finance Committee and Joint Operating Committee for review, revision and approval. A final DSRIP plan is sent to the MVHP Executive for final approval. Oversight and monitoring of the DSRIP plan is done by the MVACO CEO and NHP Chief Medicaid Officer and reported to the Executive Committee. The DSRIP funding is largely focused on supporting the MVACO programs development and operations since NHP programs are funded through the percent of premium for administration. We do not anticipate modifying that or the program oversight over time.
The MVHP will utilize DSRIP funds to develop, implement, continually evaluate and redesign integrated structures, functions, and processes of care as outlined in the goals below.
- Implement an integrated approach to population health management that includes physical health, behavioral health (BH), long-term services and supports (LTSS), health-related social services, and overall member care.
- Develop a physically integrated care management model which includes care teams from NHP and MVACO focused on impacting drivers of total cost of care • Increase member-centeredness and member experience of care by designing innovative models that engage members “where they are” and addresses health-related social needs
- Improve health information technology infrastructure by creating centralized data warehouse that houses both clinical and financial data, shared care management platform and integrated dashboards and analytics in order to provide tools and reporting to achieve ACO goals of reducing cost and improving quality of care and patient outcomes
- Increase member access to culturally and linguistically appropriate services and to medical and diagnostic equipment that is accessible to Members with disabilities
- Develop the workforce appropriately to support the interdisciplinary and decentralized model of care such as community health workers, social workers, nurse care managers, population health managers, and other roles that may be invented during the course of this program.
Initial investments in PY0 and PY1 are focused on developing the MVACO as a new organization, designating leadership, setting up new office space and integrating processes with Neighborhood Health Plan and the EOHHS contracted Community Partners. Additionally we are investing in a skilled, caring workforce to support primary care clinicians in a model of care coordination and care management for high risk and rising risk patients to complement, but not duplicate, the care management programs at NHP that target the highest risk patients. In order to implement new care processes efficiently and to have effective data and reporting to manage the ACO, we are also directing investments to health information technology in the early years, specifically for a data warehouse that will integrate clinical and financial data from multiple sources and for new connections for data and information sharing.
We believe the care management programs combined with NHP’s utilization management programs for high expense areas like home health care and pediatric inpatient utilization in high cost settings as well as new taskforces we have formed to manage emergency room utilization for example, will help us achieve cost savings even while investing in new programs. We are investing in systems and personnel such as population health managers, to assist primary care clinicians in managing quality performance as well so that we will improve patient health outcomes and care processes during the program period. Primary care clinicians are held accountable for cost and quality through the value-based payment methodology whereby they are contributing a 5% withhold on ACO claims to be held for potential deficit sharing, but in the case of a surplus, they can share in the surplus depending on achieving quality metric targets and a care retention metric. All care team members will be educated on the quality goals so that anyone working with patients can help us achieve those goals.
During the course of the five year program many of the early investments in HIT will be reduced to operating costs only, freeing up additional funding to develop innovative programs based on what we have learned from our early work and from the work of other ACOs in the state. We will be exploring telehealth opportunities to enhance access to behavioral health or other specialty care that may be limited locally, other opportunities for community based care, funding for social needs such as temporary phones, transportation or other assists, and funds for wellness grants for programs clinicians may want to start for health education or exercise classes, for example. We will also partner with local agencies doing great work to address housing and food insecurity, and fund expansion of the mobile fresh produce market already operating at the GLFHC where 67% of the population screened in for food insecurity, much higher than the state average of 10%. Last year GLFHC provided 185,000 pounds of fresh produce to 1338 unique households and we will build upon that success.
For each category of investment planned we have identified evaluation metrics. We will be tracking these on a key metrics dashboard so that we will know whether they have supported our goals as intended. One of our challenges is that we have a large number of varied investments and therefore many projects to implement and track over the first two years. Another challenge is to be able to find bilingual social workers. We plan to take advantage of the statewide investments in workforce training for community health workers, primary care loan repayment, support of the family practice residency program for additional support for our model of primary care and care management. The major challenge will be planning for sustainability as the DSRIP funding decreases over the five years. We believe we have targeted programs in certain key areas to achieve cost savings initially but that may be more difficult in the later years. We are hopeful that as we implement programs and learn new ways to deliver higher quality care at lower cost such that we achieve savings, then we will know how to implement changes in the core processes of care that will be sustainable beyond the funding period.
Website
The MVHP website is under the My Care Family name and is located at this link: https://www.mycarefamily.org. It is designed to be a resource for patients and includes the provider directory.