What is Primary Stroke Service (PSS)?
The Massachusetts Department of Public Health (DPH) initiated this program in 2002 with the goal of improving stroke care in Massachusetts. DPH promulgated licensure regulations in March 2004, which specified the requirements for a hospital to receive PSS designation. In 2019, there are 67 hospitals and satellite emergency facilities that currently have PSS designation.
Massachusetts Primary Stroke Service (PSS) designation requires a readiness to provide timely acute stroke evaluation and treatment. As part of its PSS designation, a hospital must provide emergency diagnostic and therapeutic services 24 hours-a-day, seven days-a-week to patients presenting with symptoms of acute stroke. These services are needed to ensure that every patient who arrives within hours of the start of his/her stroke symptoms and is eligible can be treated with IV-tPA. In follow up to the PSS program, a diversion plan for ambulances was created requiring the transport of patients presenting with symptoms of acute stroke to the nearest designated PSS facilities (bypassing non-PSS facilities even if they are closer).
PSS validation overview
In the spring and summer of 2019, the Massachusetts Department of Public Health (DPH) conducted on-site validation of selected PSS Facilities. The data validation focused on adherence to hospital regulatory requirements and providing support for implementing stroke care best practices.
DPH selected 21 hospitals and 3 satellite emergency facilities for a validation site visit based primarily upon facilities where a longer time period had passed since the last validation was performed.
- DPH identified up to 10 ischemic and transient ischemic strokes for on-site chart review to assess completeness and accuracy of reporting.
- When appropriate, validators provided on-site technical assistance regarding state regulations, facility policies and procedures, and PSS data abstraction and reporting.
- Facilities with room for improvement were selected for additional quality improvement coaching. Those facilities received a site-specific improvement plan and a follow up call one month later to document improvement progress.
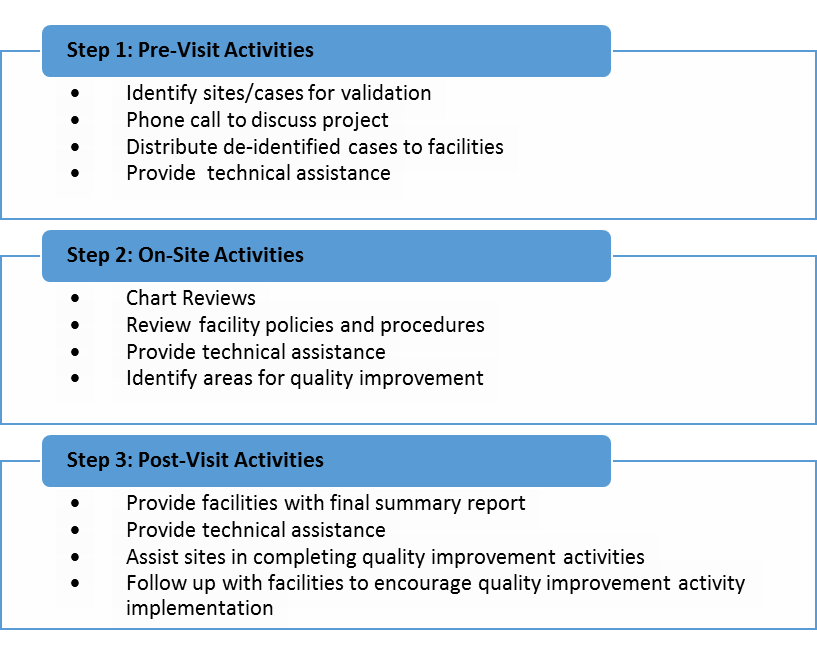
PSS Validation Project Steps
PSS data validation findings
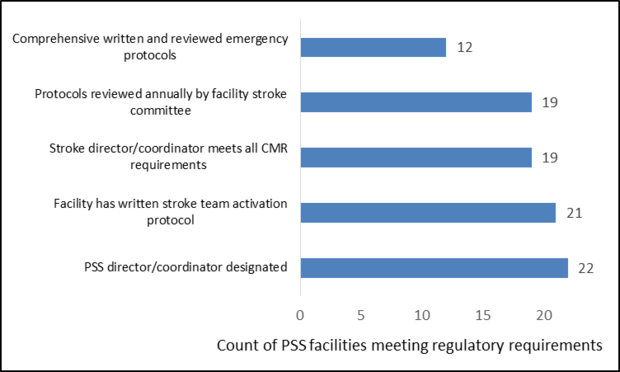
PSS requirements include comprehensive emergency protocols for facility stroke care and team activation that meet best practices. These protocols must be reviewed by the facility stroke committee on an annual basis. All PSS facilities must also have a designated stroke director or coordinator who meets annual continuing education requirements in the state regulations or as otherwise specified by the facility. Overall, DPH found that the selected facilities were compliant with hospital regulatory requirements, but identified some areas for improvement:
- Of the 24 facilities validated, 2 (8%) facilities either had no PSS director or the incumbent was leaving with no replacement identified.
- Five (21%) facilities had PSS directors or coordinators who did not meet all hospital regulatory requirements.
- Twelve facilities (50%) received recommendations to improve or create new emergency protocols, particularly protocols for increased intracranial pressure.
- Three (12%) facilities lacked a written protocol for notifying and activating the Acute Stroke Team when patients present with signs and symptoms of acute stroke.
- Five (21%) facilities had protocols that had not been reviewed by the facility stroke committee in the last year.
Validated Primary Stroke Service Facility Meeting Specific Regulatory Requirements in 2018, N=24 PSS facilities
As part of the validation visit, up to 10 ischemic or transient ischemic strokes were selected for an on-site chart review. Overall data abstraction was of good quality: validators found that 34 submitted data elements were being completed with greater than 90% accuracy when compared to the patient chart. Facilities had difficulty documenting the following data elements:
- Last known well time (82% with no discrepancy)
- Symptom onset time (86% with no discrepancy)
- Brain imaging date and time (65% with no discrepancy)
- Date and time of alteplase initiation (88%)
Technical assistance was provided whenever discrepancies were found between hospital policy and hospital regulatory requirements or data abstraction and the patient chart. This included linking PSS programs to other facilities in their hospital network for cross training and providing sample triage and treatment protocols for acute strokes. These examples were used to strengthen PSS facilities’ emergency medical services and patient treatment protocols. Technical assistance related to data abstraction included how to select patients for data entry, confirming patient CT initiation time by using the CT film, and entering cases in a timely fashion.
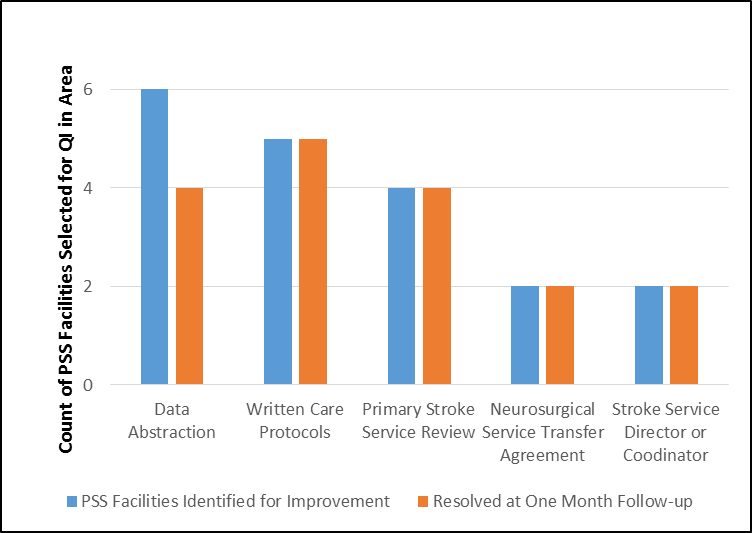
Areas Identified for Quality Improvement Activities at Selected Massachusetts PSS Facilities, N=7 PSS facilities
Beyond real-time technical assistance, validators selected 7 facilities for additional quality improvement (QI) activities based on the number and scope of regulatory and data abstraction discrepancies found and facility staff experience. Using the findings from the on-site validation, validators drafted a site-specific QI plan with items needing improvements and action items addressing each item. Validators went over the report in detail with facility staff and performed a one-month follow-up call to assess progress. QI was often recommended for data abstraction, written or improved ED and PSS protocols for stroke patients, and written transfer agreements. After one month follow up, 2 facilities needed additional time to complete all of their QI activities, however, all facilities were able to accomplish at least some of the activities.
Challenges and next steps
Many of the facilities validated had well established PSS programs with clearly defined policies and procedures and robust data submissions processes. Among facilities with less developed programs several themes emerged, including staff turnover and training, and competing work priorities. Training of PSS data abstractors was also a challenge for many facilities. Some facilities contract with a professional abstraction companies, but others use salaried employees; training and data element documentation can be inconsistent.
DPH will continue to follow up with the facilities that participated in the QI program to ensure quality care. DPH has also begun providing hospital specific data reports to all Massachusetts PSS facilities. These reports contain a section on data completeness. Additional opportunities to address facility data completeness and accuracy are being considered.
Additional Resources
-
Open PDF file, 381.39 KB, MA PSS Facilities Validation Summary (English, PDF 381.39 KB)