Introduction
Falls and fall-related injuries are common among nursing home residents with about half of all residents suffering a fall at least once a year [1]. Nursing home fall rates range from approximately 0.6-3.6 falls per bed per year, with a mean of 1.7 falls per bed per year [2]. Identifying nursing home residents at highest risk for falls can facilitate targeted intervention, potentially reducing incidence and associated costs. Using datasets from Health Care Facility Reporting System (HCFRS), CMS’s Minimum Data Set (MDS) and Payroll Based Journal (PBJ), this data brief aims to
- Describe the percentages and rates of falls with injury by age group and by priority population in Massachusetts nursing homes and trends in fall with injury over time,
- To understand how fall rate differ by resident race and ethnicity to address existing disparities and prevent widening disparities among nursing home adverse outcomes, and
- To identify facility practices and staffing that may have the greatest impact on reducing falls with injury within a facility.
Nursing Home Population 2018–2022
In 2022, 36% of the nursing home residents are 85 and older and 88% of nursing home residents are 65 and older. About 60% of nursing home residents are female.
Nursing home residents are predominantly White/ Caucasian (86.9%).
Figure1: Age of residents in MA nursing homes, 2022 MDS
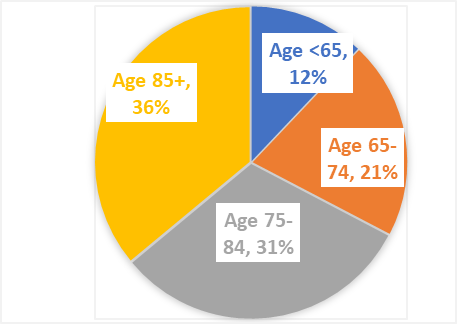
Data source: CMS Minimum Data Set, 2022
Overall, nursing home census has decreased from approximately 120,000 prior to COVID-19, to 98,000 from 2020 forward.
The proportion of the population aged 85 and older decreased (from 38% prior to COVID-19 to 36% in 2022), while the proportion of residents aged 75-84 years increased from 28% to 31% in the same time.
Figure2. Total number of residents and percent of resident by age groups, 2018-2022 MDS
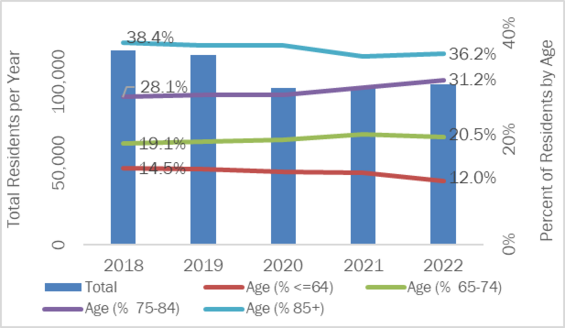
Data source: CMS Minimum Data Set, 2022
Describing the Falls with Injury that Occurred in Nursing Homes from 2018–2022
Among the 14,951 falls with injury reported to HCFRS from nursing homes in 2018-2022, most (81%) occurred in a resident’s own room. The most commonly (72%) used assistive equipment at the time of the fall were walker and wheelchair.The majority (70%) of activities occurring immediately preceding a fall with injury are: ambulating, getting out of bed, and getting up from a chair.
Figure 3: Falls with injuries by cognitive status
Finding: Among reported falls with injury, 50% occurred in residents that have Alzheimer’s Disease or Dementia.
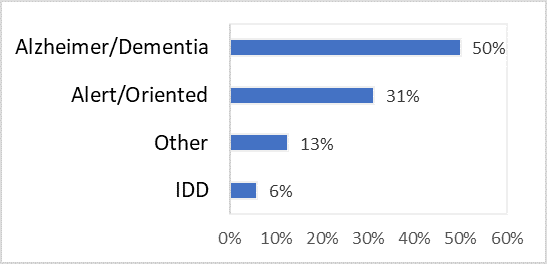
IDD: Intellectual and Developmental Disabilities
Recommendations:
Residents with dementia comprise the largest disease group of nursing home residents. A randomized trial showed that residents with cognitive impairment had a greater benefit from interventions such as to wear hip protectors and progressive balance and resistance training cognitive problems [3].
Figure 4: Frequency of falls with injury by time of day, HCRFSS 2018-2022
Finding: Falls with injury occurred with high frequency at 7am-8am and 11am--12pm during the morning and afternoon mealtimes. For the afternoon/evening shifts, fall with injuries occurred with very high frequency from 2pm to 7pm
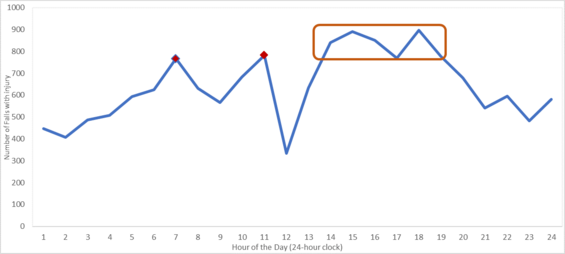
Recommendations: Facility administrators can increase staffing during residents’ mealtimes and supporting residents to meet bathroom needs. Additionally, facility administrators can consider increasing activities staff during peak fall times, as well as the development of appropriate shifts and environmental adaptions.
The trend of Falls with Injury that Occurred in Nursing Homes from 2018–2022
Figure 5: Rate of falls with injury, 2018 - 2022
Findings: The total number of short- and long-stay residents residing in nursing homes decreased from approximately 120,000 prior to COVID-19 to 98,000 in the years following.
The rate of falls with injury increased from 27.9 falls with injury/1,000 residents in 2018 to 34.8 falls with injury /1,000 in 2022, an almost 25% increase.
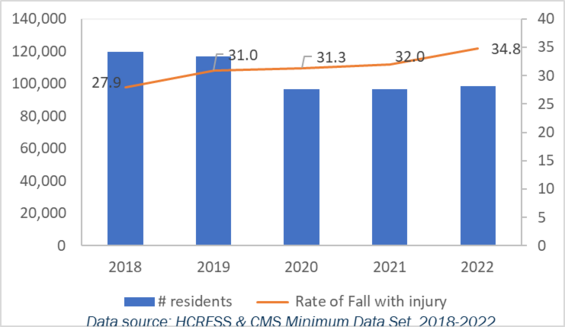
Figure 6. Rate of all with injury by race/ethnicity, MDS and HCRFS, 2018-2022
Findings: The rate of Falls with injury appears to be highest among Asian residents and lowest among Black residents across all the years. On average, Black residents are about 10 years younger than White residents which may explain why the rate of falls with injury is lowest among Black residents.
The rate of falls with injury among Black and Hispanic residents have been increasing since COVID-19 (2020).
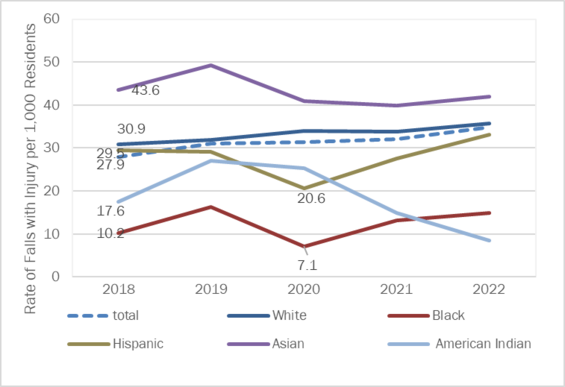
Recommendations: State policy is needed to target structural racism, socioeconomic and cultural drivers of adverse outcomes in nursing homes. Nursing homes should review their own data on falls with injury routinely, using a health equity lens.
Figure 7: Rate of falls with injury by age 2018-2022
Findings: The rate of falls with injury is highest among residents 85 years and older compared to all other age groups. This remained consistent for all the years included.
The younger age groups appear to be experiencing an increasing trend in the rate of falls with injury.
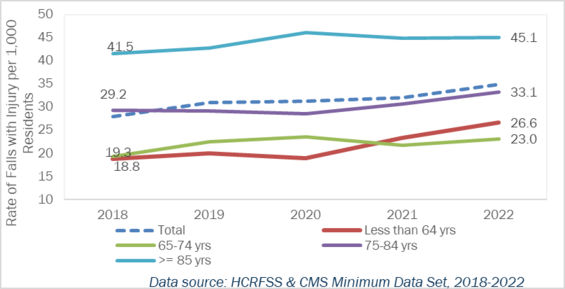
Recommendations: Currently, adults >=85 years account for 2% of the population; by 2050, this proportion is projected to increase to 5% [4]. Many fall risk factors increase with age, including chronic health conditions related to falls, increased use of medications, and functional decline[3]. More research is needed to determine how fall risk factors differ among the older residents and to identify targeted interventions that could adequately address the needs of these older residents.
Figure 8: Rate of falls with injury by staffing compliance status, 2018-2022
Findings: Beginning April 2021, DPH promulgated regulations that require facilities to provide a minimum staffing ratio of 3.508 total nurse hours per resident day. From 2018 through 2022, facilities that achieved this minimum staffing ratio consistently had a lower rate of falls with injury compared to facilities that provided less total nurse hours per resident day.
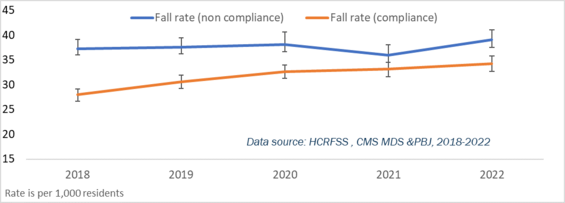
Recommendations: Facility administrators showed target resources for the staff members to improve the knowledge and skills in falls prevention. Facilities with low-source staffing should target support or investment on recruiting, training and/or retaining nurse staffing such as certified nurse aids (CNA).
Fall Prevention Resources
1. STEADI (Stopping Elderly Accidents Deaths & Injuries)
The Centers for Disease Control and Prevention (CDC) made fall prevention a routine part of clinical care. STEADI uses established clinical guidelines and effective strategies to help primary care providers address their older patients’ fall risk and identify modifiable risk factors
2. AHRQ’s Safety Program for Nursing Homes: On-Time Falls Prevention
The Agency for Healthcare Research and Quality (AHRQ) created On-Time Falls Prevention to help nursing homes with electronic medical records identify residents at risk for falls. The tools are designed to help a multidisciplinary nursing home team prevent falls that can be avoided with good preventive care.