Part 1. Executive Summary
The BACO and BMC HealthNet Plan (BMCHP) Partnership Plan’s vision is well-aligned with the Commonwealth’s seven delivery system reform goals. Our vision is to improve the health of our members by developing an integrated delivery system that provides the right care, in the right setting, at the right time. Our strategy to accomplish this includes: (1) placing members’ and their family’s needs at the center of their care; (2) keeping health local in the community and integrating healthcare with social services; (3) attending to care transitions; (4) managing performance with data; (5) innovating and iterating on programs with proven results, while keeping costs low; and (6) investing in and enabling our workforce, including affiliated physicians.
1.1 ACO Composition and Governance Structure
Boston Accountable Care Organization includes PCPs from the following groups:
- The Boston Health Care for the Homeless Program, Inc.
- Boston Medical Center Corporation d/b/a Greater Roslindale Medical and Dental Center
- Boston University Affiliated Physicians, Inc.
- Boston University Family Medicine, Inc.
- Boston University Obstetrics and Gynecology Foundation, Inc.
- Child Health Foundation of Boston, Inc.
- Codman Square Health Center, Inc.
- Dorchester House Multi-Service Center, Inc.
- Evans Medical Foundation, Inc.
- Greater New Bedford Community Health Center, Inc.
- Health First Family Care Center, Inc.
- South Boston Community Health Center, Inc.
- South End Community Health Center, Inc.
- Mattapan Community Health Center, Inc.
- Manet Community Health Center, Inc.
- Stanley Street Treatment and Resources, Inc. (SSTAR)
- Sturdy Memorial Hospital, Inc.
- Valley Health Partners, Inc./Holyoke Medical Center Inc
BMCHP is a longstanding managed care organization (MCO) under the MassHealth program. It provides a wide range of administrative functions including network management, member services, claims 2 adjudication and compliance. BMCHP is an affiliate within the larger BMC Health System and is serving as the MCO under the Boston Accountable Organization Partnership Plan.
The governance structure for the ACO Partnership Plan consists of the following:
- BMC Health System/ Boston Accountable Care Organization Joint Operating Committee
- Boston Accountable Care Organization Board of Directors
- Boston Accountable Care Organization Quality, Clinical, IT and Informatics Committee
- Boston Accountable Care Organization Finance/Budgets Committee
- Boston Accountable Care Organization Patient and Family Advisory Committee
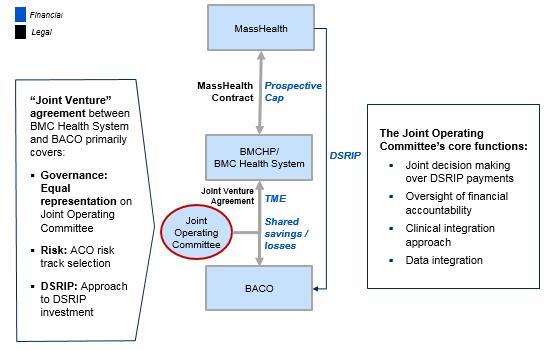
Joint Operating Committee The Joint Operating Committee (JOC) supports functional integration between BMCHP and BACO. Joint Operating Committee decisions are made “bilaterally” with both the JOC and BACO agreeing on all decisions (e.g., DSRIP investment framework). Currently, the Joint Operating Committee has six members: three of those members are representatives of community health centers appointed by BACO and BMC Health System has appointed the other three:
Susan Coakley President, Boston Medical Center HealthNet Plan
William Creevy, M.D. President, Faculty Practice Foundation
Alastair Bell, M.D. EVP, Strategy and Chief Operating Officer, BMC Health System
Cynthia Sierra CEO, Manet Community Health Center
William Halpin CEO, South Boston Community Health Center
Sandra Cotterell CEO, Codman Square Health Center
An overview of how the Joint Operating Committee fits within the BMCHP, BMCHS and BACO ecosystem is as follows:
Boston Accountable Care Organization Board of Directors
The BACO Board is comprised of 19 directors with the below composition with ACO Participants having at least 75% control of the Board.
- 6 Boston Medical Center representatives
- 6 physician group representatives
- 6 community health center representatives
- 1 consumer representative
The BACO Board is also supported by several committees.
Boston Accountable Care Organization Finance/Budgets Committee The Finance/Budget Committee provides assistance to the BACO Board in fulfilling its responsibilities with respect to its oversight of the Corporation’s finance, budget, and contracting. Specific areas of oversight include insurance plan offerings, network maximization, financial management, and standards and guidelines. There are 19 voting members with representation from each of the BACO MassHealth ACO sites.
Boston Accountable Care Organization Quality, Clinical, IT and Informatics Committee The Quality/Clinical Committee provides assistance to the BACO Board in fulfilling its responsibilities to oversee and ensure the integration of minimum standards for clinical care and patient service provided by the organization’s participating providers. There are 26 voting members with representation from each of the BACO MassHealth ACO sites.
Boston Accountable Care Organization Patient and Family Advisory Committee (PFAC) The Patient Advisory Committee provides assistance to the BACO Board in fulfilling its responsibilities to ensure representation of the interests of the ACO’s patients and consumers. BACO is currently gathering nomination recommendations from our ACO sites for participation in the PFAC.
Decision Making Decision making takes place at both the partnership level through the Joint Operating Committee and at the ACO level through the governance structure established by the bylaws of the Boston Accountable Care Organization.
The Joint Venture agreement between the Boston Medical Center Health System (“BMCHS”) and Boston Accountable Care Organization established a Joint Operating Committee to oversee the joint obligations of the Boston ACO and BMC Health System, including BMCHP, for the MassHealth ACO program. The JOC is charged with the following core functions: (1) joint decision making over DSRIP payments; (2) oversight of financial accountability; (3) clinical integration approach, and (4) data integration.
As noted above, Joint Operating Committee decisions are made bilaterally – both the JOC and the BACO Board of Directors must agree on those decisions. If there is not initial agreement between the JOC and the BACO Board, the committees will iterate until mutual agreement is reached.
1.2 ACO Population Served
According to the DSRIP notification letter dated October 31, 2017, BACO primary care sites have 111,922 attributed members. Service areas and demographics of these service areas are below. It should be noted that percentages reflect the total number of MassHealth members residing in the respective service area as of October 2017.
|
Service Area |
Average Age |
Percent Under 18 |
Percent Female |
Percent Disabled (RCII) |
Percent African American |
Percent Hispanic |
Percent Homeless |
% Non English Speaking |
|
ATTLEBORO |
28.10 |
34.88% |
52.52% |
9.84% |
6.06% |
8.93% |
0.69% |
6.88% |
|
BOSTON - PRIMARY |
29.12 |
34.92% |
51.51% |
13.71% |
42.49% |
19.98% |
2.07% |
22.76% |
|
BROCKTON |
25.93 |
40.50% |
55.39% |
8.12% |
32.72% |
9.63% |
0.61% |
14.72% |
|
FALL RIVER |
25.53 |
40.37% |
56.80% |
14.06% |
7.38% |
14.22% |
0.70% |
8.00% |
|
FALMOUTH |
29.63 |
33.96% |
55.79% |
6.95% |
5.06% |
3.60% |
1.98% |
1.77% |
|
GREENFIELD |
28.61 |
32.48% |
52.21% |
10.53% |
3.47% |
7.36% |
0.48% |
2.99% |
|
HOLYOKE |
27.15 |
34.45% |
57.57% |
20.74% |
3.30% |
57.33% |
0.40% |
21.33% |
|
LYNN |
26.26 |
37.99% |
53.74% |
8.81% |
11.66% |
29.80% |
0.70% |
33.35% |
|
MALDEN |
27.34 |
35.16% |
52.75% |
6.50% |
19.29% |
14.37% |
0.47% |
31.92% |
|
NEW BEDFORD |
27.58 |
35.11% |
58.90% |
14.11% |
8.80% |
21.90% |
0.74% |
11.20% |
|
NORTHAMPTON |
28.81 |
35.18% |
54.30% |
9.82% |
5.82% |
13.08% |
0.37% |
7.09% |
|
PLYMOUTH |
31.00 |
23.80% |
53.03% |
9.75% |
4.58% |
2.82% |
0.77% |
2.53% |
|
QUINCY |
31.43 |
27.70% |
50.71% |
9.40% |
19.72% |
5.69% |
1.11% |
16.79% |
|
REVERE |
22.23 |
52.95% |
52.50% |
6.12% |
4.93% |
47.81% |
0.55% |
54.50% |
|
SOMERVILLE |
31.11 |
24.27% |
47.86% |
7.74% |
24.79% |
7.27% |
0.94% |
12.50% |
|
SPRINGFIELD |
27.38 |
34.00% |
53.63% |
17.25% |
13.49% |
37.97% |
0.44% |
15.36% |
|
TAUNTON |
25.77 |
41.17% |
53.34% |
10.00% |
10.17% |
10.41% |
0.56% |
5.02% |
|
WALTHAM |
34.08 |
19.91% |
51.65% |
7.43% |
12.66% |
12.29% |
0.83% |
18.26% |
|
WAREHAM |
30.51 |
25.96% |
57.41% |
13.10% |
11.53% |
3.84% |
1.88% |
1.02% |
|
WESTFIELD |
28.86 |
31.16% |
55.88% |
12.68% |
2.90% |
11.00% |
0.37% |
10.66% |
|
WOBURN |
31.16 |
27.53% |
49.79% |
7.94% |
12.58% |
5.67% |
0.41% |
10.62% |
Until an analysis can be done on the needs of the full BACO population, particularly those not currently members of BMCHP, we anticipate that BACO’s BH/LTSS population characteristics will be similar to that of BMCHP’s current membership. Based on claims and pharmacy data, 35% of members have a behavioral health or substance abuse (SA) condition. Conditions driving this high prevalence are bipolar and depression (58%); personality disorders (14%) and drug dependence (14%). Condition prevalence is highest in Rating Categories II and X; 73% of members with disabilities and 88% of the CarePlus B population have a behavioral health diagnosis. Over half of members with chronic conditions including asthma, coronary artery disease, congestive heart failure, chronic obstructive pulmonary disease, and diabetes have behavioral health comorbidities. Regarding LTSS needs, approximately 10% of BMCHP’s population has a disability. For this population, 37% have been diagnosed with at least one chronic disease and 32% have a medical condition that can result in a physical disability.
One challenge we anticipate is related to patient engagement. From our MassHealth ACO Pilot experience, commonly reported challenges to patient engagement include a varied level of patient readiness to participate in care management, and an inconsistent ability amongst patients to adhere to activities in support of reaching their respective care plan goals. More specifically, issues with medication adherence, a high rate of “no shows’ for scheduled appointments, and use of emergency room as proxy for primary care and complex medical and behavioral health issues.
1.3 Overview of DSRIP Investment Approach
The Population Health Services (PHS) Division of BMCHS will have responsibility for our overall approach to population health management. PHS is dedicated to the implementation of ACO strategy and programs, including the primary-care based complex care management focusing on the top 2-3% of members, ED care management and the readmissions care team programs. These programs are complemented by local programs overseen by BACO that each practice site has identified as complementary to the PHS programs in addressing local member needs. To prevent duplication with local programs, local program leaders will be provided lists of patients enrolled in primary care complex care management.
As indicated in our RFR response, we acknowledge that our objectives may evolve over the five-year period. With that in mind, we a planning for a two-phased approach over the five year period:
|
Years 1 – 3 |
Focus on developing clinical and financial integration capabilities while simultaneously beginning to improve quality and achieve cost savings. |
|
Years 4 – 5 |
Maximize ability to focus on improving quality and achieving cost savings. |
Our value based payment approach is one of shared accountability for the total cost of care for members who are attributed or assigned to BACO’s primary care providers. We have established an opportunity for BMCHP, BACO and BACO’s sites to earn financial incentives for improvements in the cost and quality of care driven by new and existing programs and processes implemented during this program. Key goals of this shared accountability framework include:
- Incenting quality outcomes
- Increasing efficiency by moving away from fee-for-service care
- Addressing social determinants which impact health outcomes
- Aligning incentives to drive individual/practice improvements that manage costs, better health outcomes, and improve member experience
- Balancing risk and rewards across practice groups and the health system
- Continually increasing our understanding of MassHealth member cost drivers and revise process and outcome measures accordingly
- Supporting medical management activities at the central and individual/practice level in order to improve performance
- Providing timely data and analysis to individuals/practices to support process improvement
Within the BMCHP-BACO financial framework, there are three tiers of settlements on Total Cost of Care (TCOC) performance. The three tiers represent the following:
- Tier 1: Risk Share Settlement between EOHHS and BMCHP
- Tier 2: Risk Share Settlement between BMCHP and BACO
- Tier 3: Risk Share Settlement between BACO and each Risk Pod within BACO
Total Cost of Care (TCOC) Performance Accountability
Tier 1
The first tier of the settlement process occurs between EOHHS and BMCHP and will follow the risk sharing parameters as outlined in Section 4.5 of the ACO contract between EOHHS and BMCHP.
Tier 2
BMCHP will establish a Total Cost of Care Target for BACO which is consistent with the TCOC target established in the Tier 1 settlement specific to the services that are part of the contract-wide risk sharing arrangement as described in Section 4.5.C of the ACO contract between EOHHS and BMCHP. BACO will not share in any risk related to the following services: Hepatitis-C Virus (HCV), Non-HCV High Cost Drugs, CBHI, and ABA. The risk sharing parameters applied to this arrangement were shared with EOHHS on January 19th, 2018 via conference call. We are happy to review these parameters again if desired. BACO’s aggregate TCOC risk exceeds 5% of its TCOC target.
Tier 3
BACO will establish individual TCOC Targets for each of its six Risk Pods based on an agreed upon fair methodology. The existence of individual TCOC Targets for each risk pod facilitates enhanced TCOC performance engagement at the individual Risk Pod level versus an approach where TCOC surplus/deficit amounts are established at the aggregate BACO level and distributed uniformly across its participants. Similar to BACO, the Risk Pods will not share in any risk related to Hepatitis-C Virus (HCV), Non-HCV High Cost Drugs, CBHI, and ABA services. We are happy to share the risk sharing parameters for the Risk Pods in person or via conference call.
Quality Performance Accountability
Across each of the three tiers, the application Quality Modifier on TCOC surplus/deficit is consistent throughout, ensuring quality of care incentives are aligned. This means that the Quality Modifier score achieved by the ACO Partnership will apply to any surplus/deficits between BMCHP and BACO as well as between BACO and each Risk Pod.
In an effort to further align incentives around quality of care performance, the TCOC targets for BACO and each Risk Pod will have funds withheld for achievement of quality metrics. Performance will be measured at the Risk Pod level and the withheld funds will be distributed back to each Risk Pod based in individual Risk Pod performance. All withheld funds will be distributed, however, on a per-member basis, high performing Risk Pods will receive more funds than lower performing Risk Pods.
Our response included in Section 2.1 under Value Based Payment Strategy further elaborates on our shared accountability approach to total cost of care management.
To achieve our ACO goals broadly described in this section and as detailed in Section 2.2, the programs and investments we are expanding/implementing are listed below.
- Primary Care Based Complex Care Management – Locally embedded RNs and Community Health Workers provide extensive support to PCPs in caring for the highest risk patients.
- Transitions of care –Inpatient RN case manager and social worker dyads focused on improving transitions after acute hospitalization and building linkages and communications between acute and post-acute providers to and avoiding unnecessary inpatient readmissions.
- ED Case Management – Locally embeddedRN case manager focused on avoiding admissions and downstream ED visits.
- SMI / SUD treatment – Embedded services in ambulatory offices and inpatient addiction consult program.
- Disease management – Programs for members with chronic diseases that provide educational and support resources (e.g., asthma and diabetes disease managers) to help manage and control disease in the long run.
- Social determinants supports – Include community outreach coordinator, housing support specialist, enrollment specialists, and financial counselors.
- Advanced technology and analytics - Building capabilities to provide actionable information to providers and improve care for all members. This includes investing and deploying a care management platform (ZeOmega) and an analytics platform (Arcadia) to identify high-utilizing members (through risk algorithms) and better understand drivers of TCOC performance. Systems will build on current state technology capabilities (including local EMRs, high-risk identification algorithms, etc.). Includes an ADT notification system.
- Quality management – At least 1 quality improvement specialist and 1 quality navigator focused on improving quality performance and outcomes. In some cases, staff will interact directly with patients to help address gaps in care.
- Tele psychiatry – Given the BH needs of our population, we are evaluating building capabilities to see patients remotely.
- Enabling investments – To support our programs, including recruiting, training, consulting.
From a sustainability perspective, as DSRIP funds decrease over time, surplus generated under the contract will be needed to support ongoing investments. Predictability of DSRIP dollars by performance year and adequacy of capitation rate funding are the more notable challenges that we anticipate.