Vision and Strategy
The vision of the Berkshire Fallon Health Collaborative ACO is to deliver integrated, person-centered care at the right time, right place, and at the right level of intensity using best practices. To this end, we have developed several priorities that will guide our use of DSRIP funds and our alignment with EOHHS’ goals for Delivery System.
Priority 1. Create high-value, integrated provider partnerships that address Members’ medical, behavioral and psychosocial needs in a person-centered, culturally and linguistically appropriate manner. We will develop and implement Care Coordination and Care Management programs, consistent with Model A Contract requirements, that include support services to manage Members with Special Health Care Needs and those who are Behavioral Health (BH) Community Partner (CP) and Long-Term Services and Supports (LTSS)-CP eligible. We will prioritize Transitional Care Management initiatives and invest in developing the necessary infrastructure as well as flexible services that target specific health-related social needs that help Members remain in the community with the help of services and supports.
We are committed to investing in new Information Technology (IT) and infrastructure that supports primary care integration with Behavioral Health (BH), LTSS and other services across the continuum. We seek to create the ability to share data and employ decision support tools that facilitate Care Management, Care Coordination and sharing of service utilization data (e.g., real-time Emergency Department [ED] utilization) across the network. We will also invest in workforce capacity and skill sets that will be needed across our network for re-deployment of staff, as well as new and expanded roles.
Priority 2. Increase BH/LTSS integration through partnerships with PCPs, Community Partners (CPs) and Care Management staff. As both an initial implementation priority and an ongoing part of our strategic vision, we plan to invest in developing strategies to maximize the collaboration with, and contribution of, newly selected EOHHS certified BH-and LTSS-Community Partners (CPs) to meet Members’ LTSS and BH needs in an integrated manner. We will prioritize the development of work flows, best practice protocols, trainings and supports to create this integrated vision. We also plan to invest in expanding community linkages between the ACO-PP and additional providers, CPs, and social services across our service area.
Priority 3. Fund “flexible services” that address social determinants of health. The MassHealth program establishes clear expectations that ACO-PPs make investments that address Members’ social determinants of health. We will support this requirement by investing in programs that ensure that Members’ social service needs are adequately assessed through our Comprehensive Assessment and, that linkages with social service organizations are established. Based upon funding authorization by EOHHS, we will invest in services such as housing stabilization, utility assistance, nutritional counseling, and counseling and supports around instability and violence.
Priority 4. Build a foundation to expand our role in accountable care delivery. We are committed to investing in incentives that promote quality outcomes and the integration of primary care with BH, LTSS, and Care Management services at the practice level. As a provider organization that has not participated in Value-based purchasing, this is a key priority.
We will invest in activities that will help partners embrace a transition to working to achieve value-based incentives. Some steps that we see as being essential to this process include, but are not limited to: developing data infrastructure to measure and share information regarding performance; developing clinical, operational and data workflows that support value-based incentives; educating providers regarding workflows, data and value-based opportunities; and, obtaining baseline data.
We also wish to fund a learning collaborative to jointly define Care Management processes, protocols and work flows among our HCB ACO partners to develop best practices. By moving toward these activities, Health Collaborative of the Berkshires will create a strong foundation for high quality, accountable care delivery.
Priority 5. Materially improve Member experience and relationships with PCPs. We plan to invest in initiatives that increase Member awareness of available health care services and education materialsthat increase Member understanding of health care needs and services. We will promote Member access to services and Member awareness of PCP choice, thereby strengthening critical primary care relationships, which we believe will lead to improved clinical outcomes and the reduction of avoidable medical costs.
ACO Composition& Governance Structure
Health Collaborative of the Berkshires (HCB), the ACO Partner, is comprised of a network of physicians within Partnership for Health in the Berkshires, our regional Physician Hospital Organization (PHO). There are over 300 providers in primary care and various specialties associated with Berkshire Health Systems (BHS), Berkshire County community physician practices, and Community Health Programs (CHP), the regional Federally Qualified Community Health Center (FQHC).Through affiliations with BHS, a private, not-for-profit organization which includes, additional partner entities include Berkshire Medical Center (BMC), BMC North Adams, Fairview Hospital (FVH), Berkshire VNA, Berkshire Faculty Services physician practices and through a management agreement access to Berkshire Long Term Care. BMC is a full-service hospital with a Level III Trauma Center offering services from bariatric care, cancer care to wound care. FVH is a Critical Access Hospital with general acute medical and surgical care, maternity unit and our Swing Bed Program, a short-term sub-acute service for rehabilitative therapies and restorative nursing care. Through affiliations with CHP, members have access to additional primary care centers and specialty services providing health care for infants, children, adults and elders who reside in Berkshire County.
Fallon Community Health Plan, the Bidder, is a not-for-profit, independent 501(c) (3) corporation. Fallon’s breadth of experience serving beneficiaries in capitated government health care includes MassHealth, Medicare, and dual eligible programs. Fallon began serving MassHealth Medicaid recipients in 1980. Fallon received multiple awards from Medicare and Medicaid in 2006-2008 and embarked on specialized programs to serve dual eligible in 2013. Fallon’s main organizational goal, which is shared by EOHHS, is to make our communities healthy. Fallon supports our Members in a manner that is consistent with EOHHS’s approach to Medicaid managed care. Fallon offers a member-centric approach to Care Management that meets the holistic needs of the Member. Fallon has approximately 227,000 Members, of which 38,000 are MassHealth consumers.
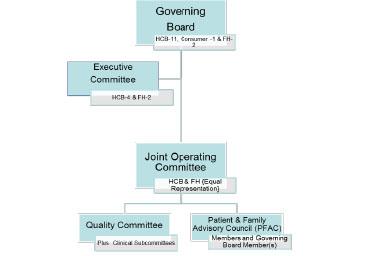
In November 2017 HCB and Fallon Community Health Plan voted to approve the organizational governance structure for the Berkshire Fallon Health Collaborative Accountable Care Partnership Plan. Please see below governance structure for
Population Served: In planning and preparation for the contract, HCB estimated there was 18,014 members in the Berkshire Fallon Health Collaborative ACO in the Adams and Pittsfield service areas of Western Massachusetts. Following HCB launch in March 2018, the actual enrollment is slightly under these projection with 15,104 Medicaid members attributed to the ACO. There are 7 additional towns that do not have unique zip codes but are part of this service area as well. They are New Ashford, Hancock, Hinsdale, Washington, Alford and Mount Washington. Our service area has a larger population of older individuals (age 45 and older) than the state and is less racially diverse with over 93% being Caucasian. Predominant languages are English and Spanish with Russian emerging. Other salient characteristics include an unemployment rate that is higher than the rest of the state and median household income and educational attainment that is lower than the rest of the state.
Berkshire Fallon Health Collaborative ACO Service Area Map
Overview of DSRIP Investment Approach
The DSRIP Plan is developed and approved by a joint work group reporting to the ACO’s Governing Board. Below highlights the high-level summary of the investment approach:
- ACO Program Strategy: Develop care coordination and care management teams to manage Medicaid members, develop disease management program to improve cost of care, integration Behavior Health and Primary Care practices, and connect Medicaid with care management hospital services with primary care practice providers
- DSRIP Goals: HCB and Fallon Health shares strategic goals to improve outcomes, reduce costs, and improve the overall quality of care for MassHealth Members. These goals are foundational to the creation of our ACO. Our shared strategic goals are to:
- Transform and innovate to improve the health status and outcomes for MassHealth Members
- Design and implement a network of high value providers who offer value over volume.
- Offer quality, patient-centered and cost-effective care that engages patients in their own health care in a culturally and linguistically appropriate manner
- Deliver integrated care including physical and BH as well as psychosocial supportsoProvide effective population health management for MassHealth Members in the Berkshire region
- DSRIP Investment Strategy: HCB DSRIP full participation plan allow Fallon Community Health Plan and the ACO to achieve three strategic objectives that align with our Model of Care. Those objectives include:
- Expand resources and capacity to allow HCB to provide care management service to the ACO population
- Assist with the creation of HCB population health model to support the unique health care and psychosocial needs of Medicaid members
- Automate system connections between Fallon, HCB, and other community partners
Anticipated Challenges: Primary challenge that concerns the ACO is the rural geography of the region and the impact it has on access to services as well as utilization rates of specific health care service lines. It is noteworthy to mention that the aforementioned characteristics make recruitment of primary care and specialty physicians extremely challenging. From a contract perspective, continuous modifications in state-wide timelines for deliverables and delays in critical information required for operation make it challenging to meet the needs of state deliverables.
Website
As of March 1, 2018, MassHealth Medicaid members were redirected to Berkshire Fallon Health Collaborative newly designed website. For more information about the contents of the site, please visit http://www.fchp.org/Berkshires.aspx.