i. A high-level description of the Consortium Entities and Affiliated Partners that comprise the CP.
The Massachusetts Care Coordination Network (MCCN) is a Long Term Services and Supports Community Partner (LTSS CP) operating in the Northern, Central and Southern regions using a Lead Agency model with strong Affiliated Partners and Material Subcontractors, all of whom have long histories within the three service regions in which we will operate. The Lead Agency is Seven Hills Family Services (under the Seven Hills Foundation provider network), and Affiliated Partners are Advocates; Brockton Area Multi Service (BAMSI); Horace Mann Educational Associates (HMEA); Boston Center for Independent Living (BCIL); and BayPath Elder Services (BayPath). A cadre of experienced Material Subcontractors in each region helps to support the work of MCCN, strengthening our ability to support specialized and hard-to-reach populations.
MCCN partner organizations are all highly qualified health and human services agencies that provide exceptional, integrated comprehensive care coordination for people who have complex lifelong needs. Care management and coordination are integral components of each Partner’s existing supports which are designed to assist individuals in pursuing their highest possible degree of personal health, well-being and independence. Each MCCN Partner currently provides care coordination with Care Coordinators/Case Managers serving as the primary liaison between the Enrollee, stakeholders, family and natural supports, treatment teams and others involved in the individual’s life (in alignment with ACO/MCO goals for care coordination). Care Coordinators provide medical, social, and support services to engage individuals in managing their health and well-being, and improve their overall quality of life. Strong community linkages to critical community resources and social service organizations provide wrap-around supports to people in our care. All MCCN partners utilize person-centered planning and self-direction models to work with each individual to meet their health care and quality of life goals.
MCCN plans to draw from its long history of supporting people throughout the state who have complex long term care needs as it partners with Accountable Care Organizations (ACOs) and Managed Care Organizations (MCOs) to provide exemplary care coordination and other supports to enhance the health outcomes, independence, and quality of life for the 4500 MassHealth Enrollees it plans to support annually.
Employing both internal and external measures and reviews, the MCCN provider organizations consistently receive top accreditations/certifications from their licensing agencies: The MassHealth Office of Long Term Services and Supports; Commission on Accreditation of Rehabilitation Facilities (CARF); The Massachusetts Department of Developmental Services; The Massachusetts Department of Public Health; The Massachusetts Department of Mental Health; The Massachusetts Department of Early Education and Care; The Massachusetts 2 Department of Elementary and Secondary Education; Massachusetts Department of Elder Affairs; The National Association for the Education of Young Children; National Commission for the Accreditation of Special Education Services, and The Council on Accreditation.
b. Community Partners Population Served
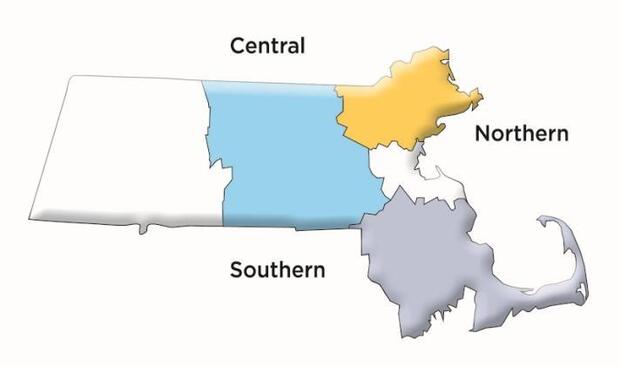
i. List the Service Areas covered by the CP. MCCN is an LTSS Community Partner operating in the Northern, Southern, and Central regions of Massachusetts.
MCCN is an LTSS Community Partner operating in the Northern, Southern, and Central regions of Massachusetts
Affiliated Partners and Material Subcontractors are community-based health care and human services organizations experienced in providing long-term services and supports to children and adults with lifelong needs in each region.
| Northern Network | Central Network | Southern Network |
|---|---|---|
| Seven Hills Family Services | Seven Hills Family Services | Seven Hills Family Services |
| Advocates | Advocates | BAMSI |
| BCIL | HMEA | BCIL |
| Mystic Valley Elder Services | BayPath | Bristol Elder Services |
| NuPath |
BCIL |
Independence Associates |
| Center for Living & Working | Road to Responsibility | |
| Elder Services of Worcester | Victory Human Services | |
| Montachusett Home Care Corporation | ||
| Springwell | ||
| Tri-Valley |
ii. Describe the demographics of the populations the CP supports or intends to support in the Service Areas covered.
MCCN has the capacity to support all MassHealth Enrollees who are eligible for long term service and support care coordination services. The partners currently support each of the priority populations, as well as infants through end-of-life care. The populations MCCN will support during this demonstration project include:
• Individuals with complex LTSS needs
• Individuals with brain injury or cognitive impairments
• Individuals with physical disabilities
• Individuals with Intellectual Disabilities and Developmental Disabilities (I/DD), including Autism
• Older adults (up to age 64) with LTSS needs
• Children and youth (ages 3 - 21) with LTSS needs
c. Overview of 5-Year Business Plan
Please provide an overview of the CP’s 5-year business plan including long term goals, anticipated challenges, and plans for sustainability.
MCCN views the Delivery System Reform Incentive Program (DSRIP) demonstration as an opportunity to introduce Managed Care Entities (MCEs) to the LTSS population and their unique opportunities and challenges. To this end, we view the ongoing collaboration of provider organizations not only within our own network, but also among the other LTSS CPs operating throughout the State that convene monthly with leadership from ADDP, as exciting platforms in which to share challenges as well as best practices. These collaborations will be part of our 5year strategy as we work to strengthen the CP/MCE relationships.
Budget Period 1 Milestones include: Development and successful implementation of the CareManager tool among all MCCN Partners; Successful contracting and relationship building with the MCEs; Development and launch of a comprehensive curriculum for care coordinator staff; Development of a comprehensive MCCN Care Coordinator policy & procedures manual; Finalization and use of a comprehensive assessment tool in line with the OLTSS tool and in concert with the other statewide LTSS CPs; Provision of LTSS educational opportunities to Care Managers at the MCEs; Meeting all deliverable deadlines and enrollment forecasts; Proven data transmission success with the MCEs and MassHealth; and Launching a truly engaged Consumer Advisory Board representative of each region.
Budget Periods 2-5 Milestones will further the overarching goal of the MCCN strategy which is to implement a creative and innovative integrated care coordination model that will improve member experience, continuity and quality of care. MCCN Care Coordination staff will work holistically with people with disabilities and chronic conditions to ensure that they have services provided to meet their personal and health care goals and daily routine needs, while improving health outcomes. Person-centered planning and informed choice will be paramount in providing supports and services that promote independence and improve access to participate meaningfully in one’s own community. Strategic opportunities in years 2-5 include: Setting baseline data in order to monitor outcomes more effectively; Developing and launching of the Transitions of Care accountability quality metric; Utilizing each Partners’ Family Support Center as a hub to communicate the availability of LTSS CP supports; Launching the full array of community connections relationships and developing these strong linkages; Demonstrating our value to the MCEs; Finalizing a sustainability plan that will be implemented post-DSRIP period; Using this demonstration to develop research projects to add to the body of LTSS knowledge through publication in journals such a s AAIDD and others; Meeting all enrollment and financial forecasting; Potential Accreditation of Case Management for Long-Term Services and Supports by NCQA; Recruiting/retaining quality workforce with diversity at all levels; Leveraging technology to develop sophisticate metrics that will be utilized to more efficiently manage population health 4 issues; Developing a robust population health dashboard; and Incorporating the MassHealth Early Notification Service when operational.
Anticipated challenges include the current shortage, both in Massachusetts and nationally, in the health and human services’ workforce and the competition among all CPs in the state who will be hiring for this demonstration project. MCCN Partner organizations offer competitive salaries and a wide range of attractive benefits in order to mitigate this challenge. In addition, MCCN will offer additional incentives by applying for the Community-Based Primary Care and Behavioral Health Workforce Initiatives: Student Loan Repayment Program and BH Workforce Development Program to attract and retain a quality workforce. The second challenge involves technology and information sharing. Most of the MCEs have developed rather standardized ways to share data such as through an STP site, which is very helpful. However, not all MCEs are approaching data sharing in a standardized way (suggesting faxing or changing methods throughout the project life). This means that Care Coordinators who already have substantial caseloads must add data manually. MCCN plans to mitigate this challenge by continued advocacy with MassHealth as well as using our software vendor, Netsmart, to work directly with the MCEs around data integration.
Once the tasks noted above are complete, MCCN’s Finance Workgroup will focus sustainability planning efforts on three key tasks:
1. Build a ‘straw model’ 3-5 year budget/cost model that includes an estimated ROI. As part of the planning phase, a significant amount of DSRIP infrastructure funds will be used to develop and implement the new care management software. The development cost is a one-time expense. The annual, ongoing PMPM expense of maintaining the software has been factored into the budget. Our sustainability model also takes into consideration that funding will be needed to key clinical staff to launch the program until such time that MCCN will engage its target number of 1500 Enrollees per region, anticipated at the end of Year Two. As the program continues to expand with the addition of Care Coordinators and other related staff, the need to rely on DSRIP funding will be largely reduced. Most of the care coordination strategies for Enrollees will focus on closing care gaps and improving care delivery across the continuum of community providers. MCCN expects transformation will result in three basic changes– expansion of ambulatory care (particularly primary care); contraction of inpatient services; and increased need for community-based and care management services. Given this focus, it is anticipated that numerous changes will occur that will impact MCCN’s caseload and resultant administrative costs and risk-based financial performance.
2. Once the ‘straw-model’ budget has been established, the Finance Workgroup will assess current resources and determine projected financial needs, including but not limited to clinical tools, systems, resources, training and infrastructure. As an early priority, MCCN is committed to finding opportunities to share resources and infrastructure, and MCCN leadership will begin early to address alignment and the potential phasing of that alignment (e.g. IT, staffing, human resources, finance, training, equipment, EHR, interoperability), share best practices and identify collective payment strategies, while providing the most effective care to Enrollees.
3. Define potential savings and other financial strategies to pursue, including payment transformation that is aligned with the State’s vision. MCCN’s long-term sustainability plan will include the shift to increased reliance on value-based payments and ACO/MCO contracts that accurately reward efficiency, value, and managing across the care continuum. We anticipate using our Statewide Investment funds for consultation around Alternative Payment Methodologies and strategy.