1.1 ACO Composition and Governance Structure
ACO Composition:
The Partnership Plan is a collaboration between the Mercy Health ACO and Boston Medical Center Health System (BMCHS). The Mercy Health ACO is comprised of:
- The Mercy Hospital, Inc. (d/b/a: Mercy Medical Center, Providence Behavioral Health Hospital and Weldon Rehabilitation Hospital), a safety-net hospital designated by the Commonwealth of Massachusetts. Mercy Medical Center is a full-service acute-care hospital in Springfield.
- Mercy Medical Group, a multi-specialty group practice with approximately 16 primary care physicians. Mercy Medical Group provides primary care to patients throughout the Pioneer Valley in two locations.
- Springfield
- East Long Meadow
- Riverbend Medical Group, a multi-specialty group practice with approximately 61 primary care physicians located in 4 locations throughout the Pioneer Valley.
- Springfield
- Chicopee
- Agawam
- Westfield
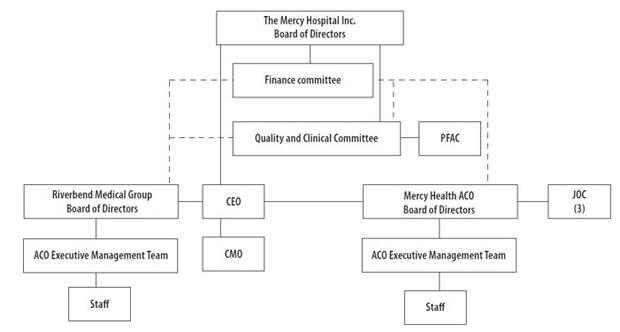
ACO Governance
Mercy’s ACO’s governance structure is in compliance with all individual requirements, including:
- Mercy ACO Board and committees have the requisite percentage and variety of providers
- Mercy ACO maintains a PFAC that includes at least one consumer, consumer advocate or community member
- Mercy ACO has a Quality Improvement Committee
Additional detail on Mercy Governance
Mercy Health ACO is an affiliate of The Mercy Hospital, Inc. and includes entities that provide a full continuum of care, including acute care, behavioral health, rehabilitation, long-term care, home care, laboratory services, end-of-life care, as well as specialist and primary care physicians (PCPs). All PCPs within the ACO are employed by an affiliate of The Mercy Hospital, Inc.
Mercy Health ACO’s Board of Directors is comprised of members of whom at least 75% are providers. These include at least one primary care provider, one mental health provider and one SUD treatment provider. Each provider member of the Board of Directors has the same voting and other rights as other Board members. The current list of Mercy Health ACO Board Members is as follows:
Mark Fulco (President)
Richard Shuman, MD
Brian Banker, MD
Daniel Weiswasser, M D
Robert Roose, MD
Mark Dumais, MD
Daniel Keenan
MCO Governance
BMCHP maintains a Board of Trustees (BOT) as its governing board. Under the corporate bylaws, the Board consists of the president of the corporate member (BMC Health System), the president of the corporation (BMCHP), a chairperson and no more than twelve (12) additional trustees. The current list of trustees is as follows:
- David Ament, Chair
- Pierre Cremieux
- James Blue
- Christopher Gordon
- Ryan Carroll
- Frank Ingari
- Susan Coakley (President, BMCHP)
- Keith Lewis, M.D. (provider)
- Sandra Cotterell
- Robert Sweet
- Stacy Cowan
- Kate Walsh (President and CEO, BMCHS)
No trustee is a consumer or consumer advocate
The BMCHP Board of Trustees is empowered to act on the following corporate matters:
- Approval of the annual capital and operating budgets or any material amendment to, or variation from, those budgets;
- Authorization of any merger or consolidation with, or any acquisition of, another corporation by the Corporation;
- Authorization of the sale, lease, mortgage, pledge or other disposition of any assets of the Corporation, or authorization of any indebtedness of the Corporation, in excess of amounts set by the corporate member or the Board from time to time
- Determination of the threshold amount of indebtedness of the corporation, over which amount authorization is required pursuant to the bylaws; and
- Approval of the filing of any voluntary bankruptcy.
With respect to decisions that may impact different affiliated or network providers (including decisions about investment strategy or the distribution of shared savings payments or surplus), the BOT would look to BMCHP’s Senior Management to make these determinations. If these provider-related decisions impacted the annual capital or operating budgets, the distribution of material assets, or the incurrence of debt, the Board would be informed and approve such actions. The Board is regularly informed of material transactions relating to providers.
Joint decision making
BMC Health System and Mercy have entered into a joint venture agreement and formed a Joint Operating Committee (JOC) that has authority to oversee the managed care program administered by BMCHP pursuant to the contract between Mercy Alliance and EOHHS. The JOC consists of 6 members, 3 of whom represent Mercy and 3 of whom represent BMC Health System. The responsibilities of the JOC include:
- Reviewing / approving budget, including DSRIP investments
- Overseeing MassHealth product performance – cost and quality
- Assessing and making recommendations on need for additional provider participants
- Providing input on areas of collaboration (network development, pharmacy benefit management, behavioral health services, community partners)
1.2 ACO Population Served
Population and Service Area:
The Mercy Health ACO’s attributed population is estimated to be ~28,000 members. Members reside in Hampden, Franklin, and Hampshire counties, with the largest number from Hampden (~96%). Initial analysis of the member cohort reveals that ~1/3 are children (under age 18) and 65% of the membership is under age of 35.
The ACO will serve a more ethnically and racially diverse population than is represented in Hampden County as a whole; Hispanic, African American, and Vietnamese members represent significant minority populations, along with a White non-Hispanic majority (~31% of the member cohort is Hispanic and 13% African American). The Greater Springfield area also is a significant destination for refugee immigrants from Africa, the Middle East and other war-torn areas, so a small but significant portion of members likely will be relatively new to the United States and the American health care systems. Eight-percent of the member cohort is non-English speaking.
The Partnership Plan has conducted initial analysis on the health attributes of the member population. While continuing to drill down into this analysis, it is important to note that The University of Wisconsin/Robert Wood Johnson Foundation "County Health Rankings and Roadmaps" shows that Hampden County has the lowest overall ranking of all 14 counties in Massachusetts in health outcomes, quality of life, health behaviors, clinical care and social and economic factors.
Challenges to serving this population
BMCHP and Mercy Health ACO foresee several challenges in serving this population:
- Maintaining adequate information. The ability to identify at-risk members and intervene in near real time is crucially important to reducing costs and achieving the best outcomes for our members. We will work over time to integrate claims, EHR, and practice data
- Improving quality of life and health behaviors. As mentioned above, the Greater Springfield area is a significant destination for refugee immigrants and Hampden County has the lowest overall ranking in health outcomes, quality of life, health behaviors, clinical care and social and economic factors.
1.3 Overview of DSRIP Investment Approach
Our goals for this participation plan are broadly aligned with (a) the goals of the MassHealth program and (b) the strategic plans of Mercy Health as we look to lead in accountable care and continue to improve both our core operations and the experience of our members.
Goals and investment strategy:
Cost and Utilization Management:
- Develop a Primary Care Based Complex Care Management (CCM) Program that targets high utilizer members (top 3%) in order to decrease costs.
- Develop an Emergency Department (ED) Care Management Program to reduce avoidable ED visits and admissions and lower costs.
- Develop a Transitions of Care Program to improve transitions after acute hospitalization.
- Create a Specialty Pharmacy Program in order to support CCM, Transitions of Care, and ED CM Programs; conduct medication reconciliation and improve medication management in order to improve health outcomes.
- Improve data and analytics capabilities to deliver actionable information that drives interventions influencing quality outcomes and TCOC.
- Ensure reliable EHR system across ACO in order to improve quality outcomes and lower TCOC.
- Creation of dedicated hospitalist program for ACO members in order to improve health outcomes.
Integration of Physical Health, BH, LTSS, and Health Related Social Services
- Incorporate BH providers into primary care practices to expand services and close gap between physical health services
- Develop in-person resources and online portal linking members with local social services in order to improve health outcomes.
- Provide digital visits (tele-health) for patients with SMI/SUD in order to improve health outcomes and lower costs.
- Create an inpatient addiction consult service in order to coordinate care for patients admitted as a result of SUD and improve quality outcomes.
Member Engagement
- Create Disease Management and Education Program in order to improve patient engagement and improve health outcomes.
Quality
- Develop a Quality Improvement Program to enhance overall quality performance and the 39 MassHealth ACO quality metrics.
Other
- Create an ACO program management structure in order to provide contract oversight, compliance, performance feedback, coaching and support in meeting TCOC and quality goals.
Our investment strategy is to make targeted investments in high-impact programs (supported by either research or our collective experience) aimed at fulfilling these goals, most importantly TCOC reduction and increased quality for our members. As DSRIP funds decrease over time, surplus generated under the contract has to support ongoing efforts.
Overall Approach to Population Health Management and Provider Accountability
Since joining Trinity Health of New England, a large regional health system, PHM strategy for Mercy ACO is being regionalized. Population Health expertise from across the regional system is being brought together under a regional clinically integrated network (CIN) that is responsible for strategy, program development, program support, data and analytics infrastructure, and contracting. The regional CIN will support local CINs, like the Mercy Health ACO, and leadership of local CINs will continue to be representative of local clinical leaders.
Accountability for performance in a value-based contract is tasked to the local CIN which is led
by a physician medical director and administrative dyad. This dyad, frequently deployed from the regional CIN, ultimately reports to the local CIN board on financial performance, quality and patient experience. The CIN dyad is also responsible to the regional board for the same metrics. Of note, the local CINs are being created as physician hospital organizations (PHOs) with equal physician and administrative representation on their respective Boards of Directors. The regional CIN management team in conjunction with the regional CIN Board of Directors (also with 50% physician representation) determine the CIN strategy for the region.
Approach to Total Cost of Care Reduction:
Part of our journey together with BMC has been using data from BMCHP as well as data provided by the State (from Mercer) to identify large and high-value TCOC management opportunities.
In order to develop a five-year business plan, the Partnership reviewed total cost of care (TCOC) data for its attributed members from both of these sources and this data was the building block for DSRIP strategy, investments, and projected outcomes.
Based on review of opportunities available in this data, the programs we intend to invest in include practice-based ambulatory complex care management, ED care management, disease management, transitions of care, homeless services, quality management & improvement and IT infrastructure.
Additionally, as noted in the PY1 budget (re)submission, BMCHP’s model of ambulatory care coordination will supplement rather than supplant Mercy’s. Mercy has had a low NVF and much of that success can be attributed to our efforts on inpatient care coordination as well as Emergency Department initiatives subsidized by the CHART Grant program. However, we have encountered challenges with respect to transitions of care due to the void in ambulatory or outpatient care management. In addition, we have not extensively invested in outpatient care coordination for this patient population. We believe the ability to utilize DSRIP funds, as outlined in this response, and overlaying the BMCHP model of ambulatory care coordination and focusing on the highest risk patients will have an impact on the frequent fliers and ultimately decrease the total cost of care.
1.4 Website
The BMCHP Mercy Alliance Website is currently under development and will be available in the coming weeks. We will share the URL with EOHHS once available.