1.1 ACO Composition and Governance Structure
ACO Composition:
Signature Healthcare Locations:
- Brockton Hospital, Inpatient, Emergency, Cardiology, Psychiatry, 680 Centre St, Brockton, MA
- Brockton Hospital, Children & Youth, Pediatrics, 680 Centre St, Brockton, MA
- Signature Medical Group, Primary & Specialty Care, 110 Liberty Street, Brockton, MA
- Signature Medical Group, Primary Care & Dermatology, 1300 Belmont St, Brockton, MA
- Signature Medical Group, Outpatient Primary Care, 130 Quincy, Ave, Brockton, MA
- Signature Medical Group, Primary Care, 166 Quincy Ave, Brockton, MA
- Signature Medical Group, Endocrinology, 176 Quincy Ave, Brockton, MA
- Signature Medical Group, Primary Care, 178 Quincy Ave, Brockton, MA
- Signature Medical Group, OB/GYN, 650 Centre St, Brockton, MA
- Signature Medical Group, Pain Management, Pre-Surgical Services, 210 Quincy Ave, Brockton, MA
- Signature Medical Group, Primary Care & OB/GYN, 360 Brockton Ave, Abington, MA
- Signature Medical Group, Primary Care, 545 Bedford St, Bridgewater, MA
- Signature Medical Group, OB/GYN, 505 Bedford St, Bridgewater, MA
- Signature Medical Group, Primary Care, OB/GYN, Pediatrics, Lab, Radiology & Plastic Surgery, 31 Roche Brothers Way, Easton, MA
- Signature Medical Group, Primary Care & OB/GYN & Lab 430 Liberty St, Suite 7, Hanson, MA
- Signature Medical Group, Primary Care & OB/GYN, 25 Warren St, Randolph, MA
- Signature Medical Group, Primary Care , Specialty Care, Rehab Services, Lab & X-Ray, 1215 Broadway, Raynham, MA
- Signature Medical Group, Primary Care & OB/GYN, 1470 New State Highway, Raynham, MA
- Brockton Hospital, Green Cancer Center, 25 Libby Street, Brockton, MA
- Signature Medical Group, Eye Services, 179 Quincy Street, Brockton, MA
- Brockton Hospital, Rehab Services, East Bridgewater YMCA, 635 Plymouth Street, East Bridgewater, MA
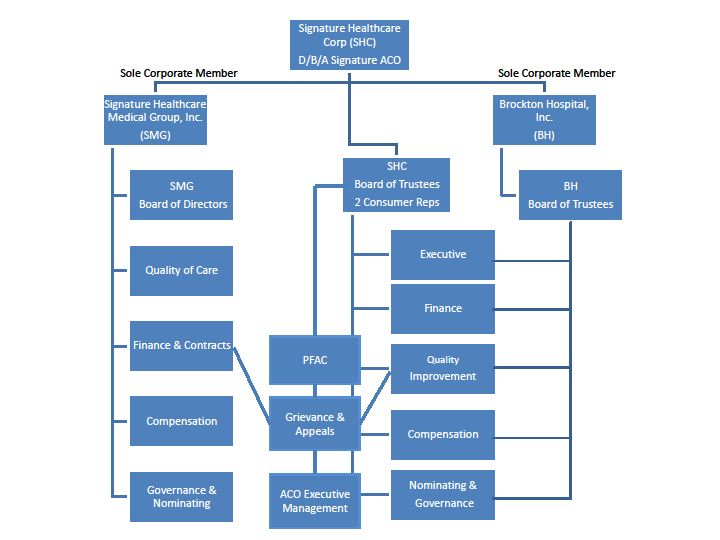
ACO Governance
Signature ACO’s governance structure is in compliance with all individual requirements, including:
- Signature ACO Board and committees have the requisite percentage and variety of providers
- Signature ACO maintains a PFAC that includes at least one consumer, consumer advocate or community member
- Signature ACO has a Quality Improvement Committee
Signature Healthcare Corporation (SHC) is managed by a Board of Trustees (BOT) consisting of 18 elected persons, and the President of this Corporation, the President of the Medical Staff of Brockton Hospital and the Chairman of the Board of Governors of the Brockton Hospital Foundation, each ex-officio with vote.
The SHC BOT is empowered to act on the following corporate matters:
| Functional Area | Responsibilities |
|---|---|
| General Functions |
|
| Organization and Authority |
|
| Fiscal |
|
With respect to decisions that may impact affiliated or network providers (including decisions about investment strategy or the distribution of shared savings payments or surplus); the BOT would look to SHC’s Senior Management to make these determinations. If these provider-related decisions impacted the annual capital or operating budgets, the distribution of material assets, or the incurrence of debt, the BOT would be informed and approve such actions. The BOT is regularly informed of material transactions relating to providers.
Additional detail on governance, specifically as it relates to population health management, is available elsewhere in this document
MCO Governance
BMCHP maintains a Board of Trustees (BOT) as its governing board. Under the corporate bylaws, the Board consists of the president of the corporate member (BMC Health System), the president of the corporation (BMCHP), a chairperson and no more than twelve (12) additional trustees. The current list of trustees is as follows:
- David Ament, Chair
- Pierre Cremieux
- James Blue
- Christopher Gordon
- Ryan Carroll
- Frank Ingari
- Susan Coakley (President, BMCHP)
- Keith Lewis, M.D. (provider)
- Sandra Cotterell
- Robert Sweet
- Stacy Cowan
- Kate Walsh (President and CEO, BMC Health System)
No trustee is a consumer or consumer advocate.
The BMCHP Board of Trustees is empowered to act on the following corporate matters:
- Approval of the annual capital and operating budgets or any material amendment to, or variation from, those budgets;
- Authorization of any merger or consolidation with, or any acquisition of, another corporation by the Corporation;
- Authorization of the sale, lease, mortgage, pledge or other disposition of any assets of the Corporation, or authorization of any indebtedness of the Corporation, in excess of amounts set by the corporate member or the Board from time to time
- Determination of the threshold amount of indebtedness of the corporation, over which amount authorization is required pursuant to the bylaws; and
- Approval of the filing of any voluntary bankruptcy.
With respect to decisions that may impact different affiliated or network providers (including decisions about investment strategy or the distribution of shared savings payments or surplus), the BOT would look to BMCHP’s Senior Management to make these determinations. If these provider-related decisions impacted the annual capital or operating budgets, the distribution of material assets, or the incurrence of debt, the Board would be informed and approve such actions. The Board is regularly informed of material transactions relating to providers.
Joint decision making
BMC Health System and Signature Healthcare have entered into a joint venture agreement and formed a Joint Operating Committee (JOC) that has authority to oversee the managed care program administered by BMCHP. JOC oversight is pursuant to the Accountable Care Partnership Plan contract between the EOHHS and BMCHP. The JOC consists of six members, three of whom represent Signature and three of whom represent BMC Health System:
| Name | Title |
|---|---|
| Susan Coakley | President, Boston Medical Center HealthNet Plan |
| Alastair Bell, MD | Executive Vice President, Strategy and Chief Operating Officer, Boston Medical Center Health System |
| Ellen Weinstein | Associate General Counsel, Boston Medical Center |
| Dr. Mitch Selinger | VP of Population Health Management, SHC |
| James Papadakos | Chief Financial Officer, SHC |
| Al Holden | Assistant Vice President Managed Care and ACO Executive Director, SHC |
Responsibilities of the JOC include:
- Reviewing / approving budget, including DSRIP investments
- Overseeing MassHealth product performance – cost and quality
- Assessing and making recommendations on need for additional provider participants
- Providing input on areas of collaboration (network development, pharmacy benefit management, behavioral health services, community partners)
- Ensure compliance with MassHealth contract requirements
- Joint decision making over DSRIP budget
- Oversight of financial accountability
- Clinical integration approach
- Data integration
1.2 ACO Population Served
Population and Service Area:
According to the PY1 notification, Signature Healthcare primary care physicians and practices currently have approximately 18,530 attributed members. Our members are disproportionately minority, low income (a majority have an annual income below $20,000) and have complex medical and social needs. Many come from families earning less than 133% of the Federal Poverty Level, struggle to make ends meet and have to deal with inadequate housing and transportation in addition to dealing with profound health needs, including, for many, living with disabilities, chronic conditions and significant behavioral health needs. Behavioral Health diagnosis is common in our population including Bipolar and depression, personality disorders and drug dependence. Condition prevalence is highest in Rating Categories II and X. Chronic conditions among our members include asthma, coronary artery disease, congestive heart failure, chronic obstructive pulmonary disease, and diabetes. In addition to chronic diseases and BH needs, our members need support managing their overall health needs including access to primary, specialty care, and community resources.
Signature ACO will serve the following Service Areas:
| Service Area | City/ Town | Service Area | City/ Town | Service Area | City/ Town | Service Area | City/ Town |
|---|---|---|---|---|---|---|---|
| Brockton | Abington Avon Bridgewater Brockton Canton East Bridgewater Easton Elmwood Holbrook North Easton Rockland Sharon South Easton Stoughton West Bridgewater Whitman | Plymouth | Brant Rock Bryantville Carver Duxbury Green Harbor Halifax Hanover Hanson Humarock Kingston Manomet Marshfield Marshfield Hills Monponsett North Carver North Marshfield North Pembroke Pembroke Plymouth Plympton South Carver White Horse Beach | Quincy | Accord Braintree Cohasset Dedham Greenbush Hingham Hull Milton Milton Village Minot North Scituate Norwell Norwood Quincy Randolph Scituate Westwood Weymouth | Taunton | Berkley Dighton Lakeville Middleboro North Dighton Raynham Raynham Center Rehoboth Seekonk Taunton |
Challenges to serving this population
Managing the Medicaid population presents some very daunting challenges. This is a population that has for many years remained disengaged with the traditional health care system, and in particular with primary care. For many in this population, use of high-cost alternatives such as emergency departments, urgent care, and acute hospitalizations has been their interaction with the health care systems currently in place. Furthermore, this population carries a higher burden of chronic conditions due to both the risk factors of social determinants of health as well as the limited access to primary care. Challenges to managing this population include how to design a health care service system that maximizes engagement of a population with pent-up demand based on chronic conditions. In designing our ACO programs for this population, we have created processes that offer the best opportunity to engage patients when they are ready. Our Emergency Room team will catch patients at a time when they are acutely ill, and will be able to update information to best locate patients when they are not in the hospital. Furthermore, this same ER team will connect the patient in front of them to the patient’s PCP. For many of these patients, they may have never seen their PCP. This opportunity will be used by our team to educate patients on navigating the healthcare system, in particular the key role that connecting with the PCP plays. We have also put in place care teams in the outpatient settings who will manage patients similarly. Our pharmacist and pharmacy techs will also play a key role in mitigating the often confusing array of medications that patients with multiple chronic conditions face. We believe that with these and other ACO programs in place, we will be better able to manage this population going forward.
1.3 Overview of DSRIP Investment Approach
Our investment approach will support our ACO’s overall performance and strategy in several important ways.
A central component to this strategy is executing on our population health management program. This program will be overseen and managed by the VP of Population Medicine, ACO Medical Director, Clinical Director of Population Health Management, as well as the Chiefs of Internal Medicine and Family Practice. This team is responsible for implementation of the ACO strategy and population health management programs, which includes primary-care based complex care management focusing on the top 2-3% of members and the Transitions of Care (ED) care team programs. We will ensure provider accountability for these programs through a combination of financial and quality incentives as further outlined below.
These programs are complemented by local programs overseen by Signature Healthcare and which each practice site has identified as important to addressing local member needs. To prevent duplication with local programs, local program leaders will be provided lists of patients enrolled in primary care complex care management.
Our DSRIP investment strategy is to make targeted investments in high-impact programs (supported by either research or our collective experience) aimed at fulfilling our overall goals, most importantly TCOC reduction and increased quality for our members. During the first three years, our focus will be on clinical and financial integration of the program, while at the same time increasing quality for our members and moving toward total cost of care reduction. In the last two years of the program, we expect surpluses generated through ACO operations to enable us to maximize our ability to continue improving quality and achieve cost savings.
We will leverage DSRIP funding to achieve ACO goals as outlined in this section and detailed in Section 2.2, by newly implementing or expanding the following initiatives:
- Complex Care Management – Locally embedded RN case managers, Social Workers and Community Health Workers will provide extensive support to PCPs in caring for the high risk population.
- Transitions of Care (ED) – Inpatient RN case managers will be focused on decreasing unnecessary admissions and readmissions.
- Pharmacy Care Management – Pharmacists and Pharmacy technicians embedded in the ambulatory offices will be focused on medication reconciliation, patient education, compliance, as well as provider education.
- Substance Abuse Disorder Team – This program will provide Office Based Addiction Treatment (OBAT) via customized treatment plans designed to fit the patient’s individualized plan; and will include an Addiction Director, OBAT Physicians, RN, Medical Assistant and Medical Office Clerk
- Behavioral Health Management Team – A Psychiatrist will manage complex psychotropic medications for the ACO population and include a Tele Pysch NP who will provide BH services digitally, including direct patient care, documentation, collateral and collaboration with on-site providers.
- Chronic Disease Management – Programs for members with chronic diseases that provide educational and support resources (i.e., NPs, RNs, Interpreters and CDEs) to help manage and control disease over time.
- Advanced technology and analytics – Building capabilities to provide actionable information to providers and improve care for all members. This includes investing and deploying a care management platform (ZeOmega) and an analytics platform (Arcadia) to identify high-utilizing members (through risk algorithms) and better understand drivers of TCOC performance. Systems will build on current state technology capabilities (including local EMRs, high-risk identification algorithms, etc.). Includes an ADT notification system.
- Quality Management – includes a Quality RN, Quality Manager and a Community Health Worker who will oversee the clinical and operational quality performance for the ACO. In some cases this staff will interact with patients to help address gaps in care.
The fore mentioned programs are critical to the success of the ACO as we begin to manage this very challenging population. In order to maintain high quality care while at the same time bend the cost curve, these programs will have to be successful. These programs will be the foundation for a strong ACO.
There will be challenges for the above programs as well. As we work to address not only the clinical conditions for this population, but also the social determinants of health, we may find that resource ratios may need adjustments. As we learn the population’s baseline it will be important to tailor these programs in order to meet the specific needs that the population demands.
Approach to Total Cost of Care Reduction:
Part of our journey together with BMC has been using data from BMCHP as well as data provided by the State (from Mercy) to identify large and high-value TCOC management opportunities.
According to the data provided by MassHealth, Signature’s PMPM is 4% below the market for RY18 with a variance of $22.18 PMPM. Adults (RC I, II, IX, X) drove 70% of this variance (~$15 PMPM) and Children (RC I & II Child) drove 30% of the variance ($7 PMPM). Predominant areas of opportunity include Lab & Radiology and IP behavioral health.
However, in working with BMCHP we have identified additional areas of TCOC reduction and we believe there is still opportunity across other programs.
Using data from BMCHP we have identified target areas for cost of care reduction, which are weighted toward pharmacy, inpatient, and BH spend as well as physician services (inpatient services, as the highest category of spend are expected to be impacted early by high risk case management, transitions of care and ED case management and are part of our initial investment focus). We are confident in our strategies for reducing total cost of care. The numbers estimating total medical expense (TME) for Signature in this population already show good management. We feel that with implementation of the planned programs we should be able to further improve our already low TME for this population.
As indicated in our RFR response, we acknowledge that our objectives may change over the five-year period. Initial performance drivers are expected to be high risk case management, transitions of care and ED case management and will be given more initial focus for implementation and management efforts. Over time, data driven improvement work across multiple elements of care will supplement these early performance drivers. This will include improvements in the management of serious mental illness, substance abuse, and social determinants of health. Due to the complex nature of these problems, improvements are expected to take longer. The analytics systems are new investments for the ACO that will marry data from multiple partners including BMCHP, Signature Medical Group, and our Community Partner’s. Through the use of the Arcadia data and analytic system and case management tools in ZeOmega’s Jiva™ system (discussed in more detail below), we will continually monitor performance and ROI of these programs with a focus on ensuring they impact cost and quality of care sufficiently and sustainably over the contract. While we will implement all programs with the goals of reducing total cost of care and increasing quality for our members, we expect that savings will scale over time.
With regard to provider accountability, the ACO leadership are financially incentivized to improve performance based on the organization’s retirement plan which will make an employer contribution to employees’ 457 plan based on lowering total medical expense (TME).
The providers will be incentivized based on quality metrics aligned with ACO’s quality metrics. Specifically, Signature’s physician compensation is aligned with the following ACO quality metrics: #5- Tobacco cessation, #8- HTN Control, #9- Diabetes Control. Over the next years, we intend to further incentivize physicians for additional quality metrics relating to ACO quality metrics.
From a sustainability perspective, as DSRIP funds decrease over time, surplus generated under the contract has to support ongoing investments. Predictability of DSRIP dollars by performance year and the adequacy of capitation rate funding are the more notable challenges that we anticipate.