Steward Medicaid Care Network, Inc (SMCN) is participating in EOHHS’ ACO Program as a Primary Care ACO called Steward Health Choice. This summary outlines Steward Health Choice’s ACO composition, governance structure, population served, our program goals, and our approach to Delivery System Reform Incentive Payment (DSRIP) investments to achieve our goals.
1.1 ACO Composition and Governance Structure
ACO Composition: Steward’s Primary Care ACO, Steward Health Choice, includes primary care providers (PCPs) from across the Commonwealth, including the northern, southern, central, and Boston regions. Steward’s network of employed and affiliated PCPs form the core of our nationally-recognized model of integrated health care delivery. Steward’s network in Massachusetts also includes specialists, who closely coordinate care for Steward Health Choice members with their PCPs. Among the largest groups in Steward’s Massachusetts network is Steward Medical Group (SMG), our physician-led, multispecialty practice organization of employed physicians. In addition to these employed providers, our network features diverse affiliates with significant experience in delivering healthcare to Medicaid patients. Affiliates include nine community health center sites, Cape Cod Health Network, nearly one hundred providers in central Massachusetts, and a multitude of independent primary care provider affiliates across eastern Massachusetts, with several large pediatric practices in the Fall River, North Shore, Methuen, and Newburyport communities. Many practices have been engaged and supportive in early planning and development of our ACO program, helping to ensure we are positioned for success with respect to health outcomes, quality, and total cost of care management.
As a Primary Care ACO, Steward Health Choice members will have access to any provider in MassHealth’s full network for specialty care and hospital services. In addition, Steward’s nine Massachusetts hospitals across ten campuses will participate as Affiliated Hospitals: Saint Anne’s Hospital in Fall River, Holy Family Hospital in Methuen and Haverhill, St. Elizabeth’s Medical Center in Brighton, Norwood Hospital in Norwood, Carney Hospital in Dorchester, Good Samaritan Medical Center in Brockton, Nashoba Valley Medical Center in Ayer, Morton Hospital in Taunton and New England Sinai Hospital in Stoughton.
Governance Structure: The Steward Medicaid Care Network (SMCN) Governing Board meets all Medicaid requirements set forth in Section 2.1.A of the Primary Care ACO contract, and will ensure the ACO program achieves its goals. Providers play a prominent leadership role throughout the governance structure. Providers on the SMCN Governing Board include physician leaders who deliver care to Medicaid patients within the ACO. These physician leaders provide clinical integration and quality improvement expertise and will inform our provider and beneficiary engagement strategies for the Medicaid ACO. Executive leaders serving as designees of providers bring financial, analytic, care management, contracting, policy, strategy, and operational expertise to Board discussions in addition to
DSRIP ACO Full Participation Plan (Attachment A) 10/24/2018 representing their designated providers’ perspectives.
SMCN established a 13-member Governing Board. All members of the Board are voting members, including our consumer advocate. Providers or their designees control 100 percent of the Board, when excluding the consumer representative from the numerator and the denominator. The Board is a balanced, diverse team that reflects our network composition with community health centers, pediatricians, and behavioral health represented.
The Board is informed by recommendations forwarded by its working committees, including the Operations, Quality, and Funds Flow Committees. The Board is responsible for oversight and strategic direction of the Medicaid ACO, including its DSRIP investments. The Board will provide oversight and direction for the organization, including but not limited to processes to promote evidence-based medicine, patient engagement, quality and cost reporting, care coordination, distribution of shared savings, and establishing clinical and administrative systems and compliance programs.
The SMCN Governing Board also established a Patient and Family Advisory Committee (PFAC) and a Community Partner Advisory Group. The PFAC will provide the perspective of patients and their families on their experience with Steward Health Choice to the Governing Board. The Community Partner Advisory Group provides input to the Governing Board regarding the development and implementation of MassHealth’s Community Partner program. This advisory group is comprised of mental health and substance use disorder treatment providers, long term services and supports providers, and providers of services that support social determinants of health. The Community Partner Advisory Group also includes primary care providers and representatives from hospitals to facilitate discussion across the continuum of care.
1.2 ACO POPULATION SERVED
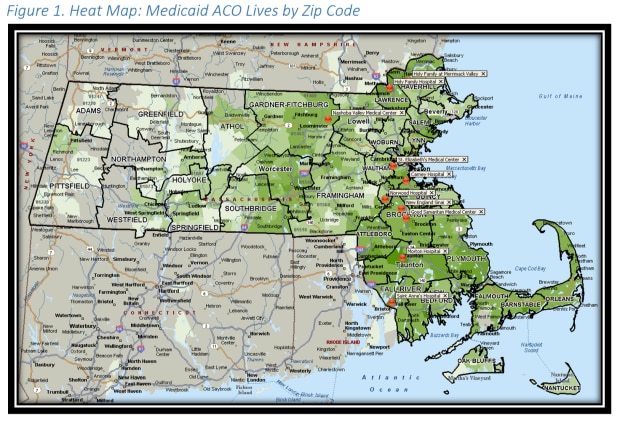
Based on the DSRIP Performance Year 1 Funding Notification Letter and preliminary enrollment data through the special assignment process, we anticipate serving between 110,000 and 145,000 ACO members, predominantly residing in eastern and central Massachusetts, as illustrated in the heat map (Figure 1) below. This DSRIP plan is built assuming membership of 133,640, per our PY1 notification letter.
Description of the member population and community
Steward has developed an understanding of the characteristics and predominant needs of our anticipated member population in the full-scale ACO program based on claims data for the SMCN ACO Pilot program, publicly available population health data, and community needs assessments for the service areas Steward anticipates serving.
Steward expects to serve a diverse member group based on the population prospectively enrolled in SMCN’s full scale ACO program as of February 2018. Members will include:
- Non-disabled children, who represent an estimated 42 percent of the population,
- Children with disabilities, who will represent an estimated four percent,
- Non-disabled adults, who will represent an estimated 44 percent, and
- Adults with disabilities, who will represent an estimated 10 percent.
Steward expects to serve a highly diverse population. Based on SMCN’s ACO full scale membership, Steward anticipates that the population’s age and gender mix will approximate the distribution shown in the table below:
Table 1: Age and gender projection
| Adults | Children | Total | |
| Female | 29% | 22% | 52% |
| Male | 25% | 24% | 48% |
| Total | 54% | 46% |
Steward also anticipates serving a racially and ethnically diverse population. Based on data from SMCN's ACO selective assignment member roster, Steward anticipates membership distribution in line with the mix shown in the table below. With improved data collection infrastructure and methods, Steward expects to reduce the “Unknown” data.
Table 2: Race and ethnicity projection
| White |
Black (nonHispanic) |
Hispanic |
Asian/Pacific Islande |
American Indian/Native Alaskan | Unknown |
Other |
|
| % Total | 45.5% | 7.7% | 5.6% | 1.9% | 0.5% | 36.9% | 1.9% |
Statewide, more than 20 percent of Massachusetts’ residents identify a language other than English as the primary language spoken in their home.1 The most common primary languages reported by SMCN ACO pilot program members are English, Spanish, Vietnamese, Portuguese, Haitian/Creole, Chinese, and Arabic.
The correlation between health status and socioeconomic background is well documented. Race, income level, educational attainment, and other social determinants are among the best predictors of health outcomes and health status. Given the low income level of the Medicaid population, many members face health-related challenges associated with poverty, including but not limited to: lack of stable housing and employment, low levels of educational attainment and health literacy, limited access to affordable healthy foods, and limited opportunities for physical exercise. Steward’s understanding of the impact of these factors on health outcomes will inform the ACO’s strategies for improving the quality and cost of member care through initiatives that seek to address the underlying public and environmental health concerns that most affect this population.
1.3 OVERVIEW OF DSRIP INVESTMENT APPROACH
ACO Programmatic Strategy Overall approach to population health management and provider accountability: Steward’s approach to population health is grounded in the principles of the quadruple aim of improving patient outcomes, decreasing total cost of care, improved patient experience, and improved provider experience. Our Population Health Management (PHM) strategy focuses resources on patients and populations where we can make the most impact on utilization and outcomes, and is driven by data and analytics.
Steward continually engages commercial payers, Medicare, and Medicaid to shift fee-for-service reimbursement and payment incentives to global, risk-based arrangements. Such contractual arrangements and incentives have led to better patient care coordination, lower medical spending over time, and an increase in the integration of our ACO resources. Steward expects to leverage its significant experience in risk-based alternative payment models, including commercial, Medicare and our Medicaid ACO Pilot, for our Primary Care ACO.
Steward has a range of metrics and methodologies used to drive performance. Steward’s program is implemented at the provider level wherever possible.
Our overall goals, to evolve from a fee-for-service reimbursement model to a global, risk-based model, are shared across payers and contracts. The value-based program for primary care providers leverages the following core principles:
A single Steward performance program that drives quality, cost efficiency and patient experience;
Measures, targets, and incentivizes that align across all Steward providers;
Incentive payments that relate to providers’ most recent performance; and
Balance between methodological fairness and operational simplicity, with an overall objective of programmatic effectiveness.
Overall approach to total cost of care management and path to sustainability: Financial sustainability is a key focus in developing our programmatic approach and in targeting our DSRIP investments. We plan to primarily use DSRIP to fund one-time investments in PY0-PY2 and minimize where possible our reliance on DSRIP funds to support the ongoing operations of the ACO program. In addition, many PY0 investments are for expenses that will be covered by administrative funding after the operational start date.
All initiatives that we implement and test in the early years of the program will be designed to be sustainable within an operating budget comprised of administrative revenue and projected performance revenue through achieving quality and efficiency targets. Long term, our sustainability in the Medicaid ACO will also be grounded in maintaining a balanced portfolio of multiple risk-based arrangements across all payers.
Vision and Strategy
Our vision for our Medicaid ACO program aligns closely with MassHealth’s stated goals, and reflects Steward’s overall mission. Through this program, we aim to:
- Deliver world-class health care where members live;
- Advance the Quadruple Aim: improve members’ health, while improving member experience and quality of care, reducing total costs and improving providers’ administrative burden;
- Actively engage a continuum of providers to address the needs of the communities we serve, including physical health, preventive care, behavioral health, and long-term services and supports;
- Create and operate a scalable, sustainable, and replicable model that uses sophisticated incentives to engage and align priorities among both ACO providers and members; and
- Use data and technology to effectively identify needs of both members and practices and efficiently target resources to meet these needs.
Our five-year plan below lays out twelve specific goals that extend this vision and that will support our efforts to improve quality and reduce total cost of care.
Cost and utilization management
- 1. Reduce avoidable ED utilization
- 2. Reduce avoidable hospital admissions and readmissions
- 3. Reduce impact of homelessness and housing instability
Integration of physical health, behavioral health, LTSS, and health-related social services
- 4. Integrate behavioral health resources into every primary care practice
- 5. Integrate and manage long-term services and supports so members remain in the community
- 6. Decrease prevalence of substance use disorder, including opioid use and incidence of overdos
Member engagement
- 7. Keep care local and community-based
- 8. Increase member engagement in primary care, preventive services and self-management
Quality
- 9. Increase prenatal care initiated in the first trimester
- 10. Improve member experience in understanding, accessing, and receiving services
Other
- 11. Develop the workforce necessary to successfully meet needs of the Medicaid ACO population
- 12. Establish a scalable, sustainable, and replicable ACO model
We developed initial goals informed by data on our Medicaid ACO pilot population. We will establish specific, measurable targets for each goal as specific data about the costs and utilization patterns of our ACO members becomes available. We will continually use data to focus and drive the programs we implement and the populations we target. We will submit requests to modify these goals and our investment strategy if, during the course of the program, our data suggests we need to adjust our focus to achieve success in managing total cost of care and quality.
1.4 WEBSITE
Steward developed the Steward Health Choice website (https://stewardhealthchoice.org/) to communicate with members and their families. The site offers a Google translate function for our diverse population to view the content in preferred languages. The site includes a short video explaining the new health plan and member FAQs to address common questions. Members can download a copy of the Member Handbook, search for a Steward PCP, and access other useful information on the site. The site directs members to contact our Member Services Call Center for further assistance understanding the health benefits and resources available to them as part of Steward Health Choice.