1.1 ACO Composition and Governance Structure
Along with carrier partner Fallon Health, the Wellforce Care Plan network includes physicians and other healthcare providers from, or affiliated with Lowell General Hospital, Lowell Community Health Center, Hallmark Health, Lowell General Physician Hospital Organization, Tufts Floating Hospital for Children, Tufts Medical Center, New England Quality Care Alliance (NEQCA), and preferred local hospitals and providers of ACO physicians.
The governance structure of the Wellforce/Fallon Health (Fallon) ACO Partnership Plan (ACO-PP) satisfies the requirements of the Model A Contract §2.3.A.1.
1.1.1 Wellforce/Fallon ACO-PP Governing Board (the ACO Governing Board):
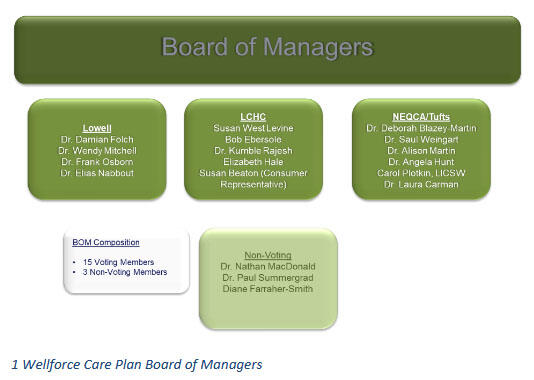
The ACO’s governance structure of the Wellforce/Fallon Accountable Care Organization Partnership Plan (ACO-PP) Governing Board has been established to meet the requirements stated in the Model A Contract §2.3.A.1. The ACO-PP Governing Board’s structure includes the requisite 75 percent provider or provider-controlled representatives and one Consumer Advocate, all of whom are voting members of the Board.
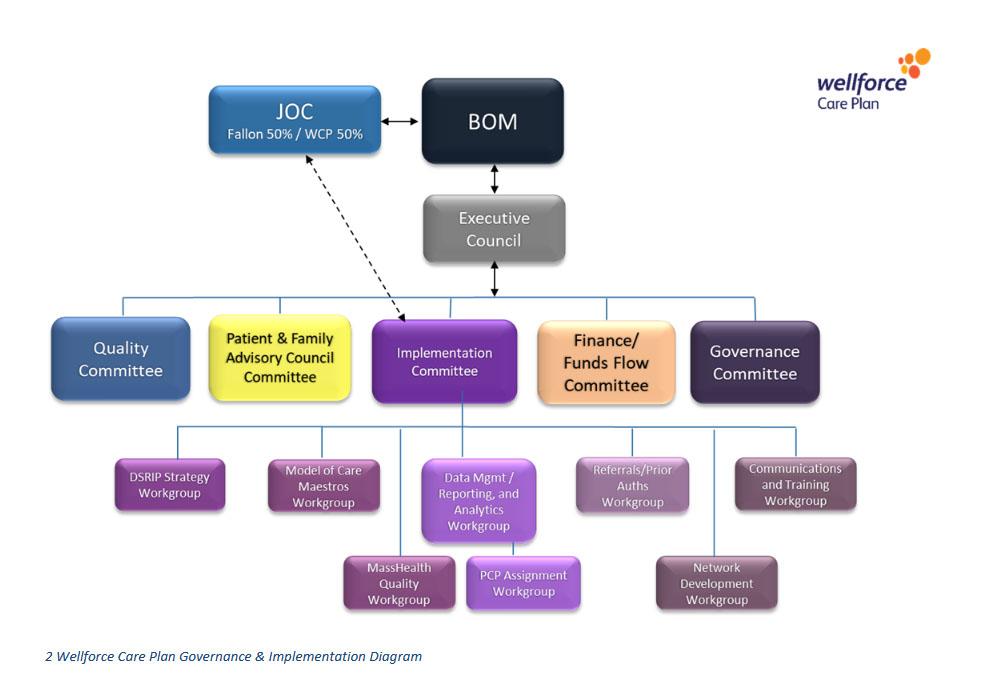
The ACO-PP Governing Board is responsible for executive-level decision-making, including decisions recommended by an ACO-PP Joint Operating Committee (JOC), decisions regarding the DSRIP plan, and decisions that may affect—financially or otherwise—different Network Providers or the ACO-PP’s financial condition (e.g., how to direct respective investment strategies or how to distribute Shared Savings). The JOC will serve as the joint decision-making body for recommendations to the ACO-PP Governing Board regarding strategic issues, including distribution of DSRIP funding, shared savings or penalties, and the ACO-PP’s overall financial condition. A Patient and Family Advisory Council (PFAC) will report to the Governing Board and, when appropriate, will provide input to the JOC.
1Wellforce Care Plan Board of Managers
The JOC is composed of twelve (12) members, six (6) members selected by the ACO Governing Board and six (6) members selected by Fallon. Of the 6 members selected by the ACO Governing Board, 2 will be representatives of the Lowell General Physician Hospital Organization (LGPHO), 2 will be representatives of the Lowell Community Health Center (LCHC), and 2 will be representatives of the New England Quality Care Alliance (NEQCA) (including the Hallmark Heath Physician Hospital Organization (HHPHO) and Tufts Medical Center (TMC). In addition, there will be one (1) to two (2) non-voting hospital representatives selected by the Governing Board.
The JOC is responsible for oversight of a master implementation work plan that will address all deliverables under the Model A Contract. During the initial implementation, the JOC has developed and monitored the execution of key implementation plan deliverables based on timelines, with an eye toward timeliness and quality of such deliverables. Following the implementation phase, the JOC will manage operational issues, ongoing care delivery and Care Management services, measurement and reporting deliverables, among other requirements, to ensure that the ACO-PP is meeting all requirements.
A Quality Committee will report to the JOC and, when appropriate, will provide input to the ACO-PP Governing Board. The authority for this structure to satisfactorily meet the requirements of the Request for Responses (RFR) derives from the composition of the JOC. Specifically, the RFR states that “the Contractor/Managed Care Organization (MCO) Partner shall designate, at a minimum, a Senior Vice President of Contracting and/or the MCO’s Chief Medical Officer who will dually report to the MCO Governing Board.” This duality provides the requisite accountability between the Contractor and the State once the ACO-PP and its governance structure is operating. Wellforce and Fallon has jointly developeda Joint Operating Agreement that will provide details regarding the operational relationship and accountability of each entity to each other and to the ACO-PP, and which outlines Fallon’s and Wellforce’s specific operational responsibilities.
In addition to the above governance structures, several key workgroups are actively deployed under the Implementation Committee (see Figure 2).
2 Wellforce Care Plan Governance & Implementation Diagram
The DSRIP Strategy Workgroup’s purpose is to define and frame the intra-WCP approval process for proposed DSRIP-funded resources for each of the PY0, PY1, rollover budgets and final 5-year plan; to make recommendations for the programmatic DSRIP funding investments; to prepare the DSRIP submissions to MassHealth, tracking expenditures, oversight, and ensuring that resources have been secured per approved DSRIP plans. The future focus of this Workgroup will be on DSRIP program evaluation.
The Model of Care Maestros Workgroup’s purpose is to serve as the lead group that will work out the details of Model of Care, including behavioral health operations, care management platform, Community Partners, and quality measures, policies, workflow, and deliverables.
The MassHealth Quality Workgroup’s purpose is to plan education, implementation of quality measures at practice level and to plan, coordinate and implement monitoring and reporting of the ambulatory quality measures in office/clinic setting.
The Data, Reporting, and Analytics Workgroup’s purpose is to ensure data integration with Fallon (to the extent permitted under applicable privacy and security laws) in order to support/drive ACO performance; to develop and distribute internal performance reports under the Model A contract; to facilitate the development of workflows critical to reporting and analytics on PCPs’ performance on cost and quality measures; to collaborate with Fallon to define the process for providing PCP claims and enrollment information about Enrollees; to facilitate intra-WCP technological interoperability; and to integrate strategic technological exchanges where necessary; and to develop and implement the daily process of PCP assignment.
The Referrals/Prior Authorizations Workgroup’s purpose is to ensure coordination of basic ACO/MCO operations including but not limited to prior authorizations and referrals; Network build out and contracting; developing workflows that foster streamlined communications amongst Fallon, WCP, and participating hospitals.
The Network Development Workgroup’s purpose is to track preferred providers, identify and resolve service area gaps, connect with Beacon on BH contracting as needed.
The Communications and Training Workgroup’s purpose is to develop strategies around WCP member and provider engagement, education, patient outreach; provider training and implementation; develop brand identity and marketing strategies, connect and align internal clinical training with overall provider training and education.
1.2 ACO Population Served
The ACO must provide the number of members attributed to the ACO, as provided in Section I of the ACO’s PY1 DSRIP Funding Notification Letter, and the Service Area(s) for which the ACO is contracted (Accountable Care Partnership Plans, only). Additionally, the ACO must provide an assessment of the populations and communities that the ACO will serve, highlighting: (1) any unique characteristics of the ACO’s population, such as demographic composition, breakdown of disease burden, etc.; (2) an assessment of population-and community-specific needs; and (3) any challenges the ACO anticipates in serving this population. EOHHS is not asking or requiring the ACO to conduct a formal Community Health Needs Assessment. Rather, EOHHS is seeking a descriptive overview of the population and the general needs.
There are 53,637 members in the Wellforce ACO in the Framingham, Waltham, Beverly, Haverhill, Lawrence, Lowell, Lynn, Malden, Salem, Woburn, Boston Primary, Quincy, Revere, Somerville, Attleboro, Barnstable, Brockton, Falmouth, Orleans, Plymouth and Wareham service areas. Our Service area varies widely in terms of age, race, ethnic and language diversity as well as other salient characteristics such as median household incomes and prevalent health conditions. Unique characteristics of our population include the population served by the Lowell Community Health Center, in which one out of four are foreign-born.
Specific challenges that the ACO anticipates in serving this population include engaging the homeless populations in our Service Area, facilitating access to behavioral health services for our pediatric members (nearly half our membership) due to pediatric provider shortages across our Service Area, and supporting the several communities in our Service Area that are disproportionately impacted by the opioid epidemic.
1.3 Overview of DSRIP Investment Approach
Programmatic Strategy: Our vision is to deliver integrated, person-centered care at the right time, right place, and at the right level of intensity using best practices. To this end, Wellforce and Fallon Health have developed several priorities that will guide our use of DSRIP funds and our alignment with EOHHS’ goals for Delivery System:
- Priority 1: Develop high-value, integrated provider partnerships that address Members’ medical, behavioral and psychosocial needs in a person-centered, culturally and linguistically appropriate manner.
- Priority 2: Increase BH/LTSS integration through partnerships with PCPs, Community Partners (CPs) and Care Management staff.
- Priority 3: Fund “flexible services” that address social determinants of health.
- Priority 4: Build a foundation to expand our role in accountable care delivery.
- Priority 5: Materially improve Member experience and relationships with PCPs.
ACO Approach to Population Health Management, Provider Accountability, Total Cost of Care Management, Path to Sustainability: Wellforce will use a population health management tool and care management platform to monitor and manage the entire membership and to identify areas at the Wellforce, hospital, regional, practice, and clinician levels that can be improved through intervention. Wellforce’s effective targeting and intervention strategy is comprehensive: the strategy is built on a primary care foundation that utilizes care management teams, community partners, and patient-centered programs with a focal point of the strategy designed to decrease unnecessary ED and inpatient utilization by the top 5% of our sickest patients. This approach was designed to bend the cost curve and set the ACO on the path to financial sustainability after grant funding tapers down and eventually expires.
Goals for DSRIP Program:
- Integrating physical health, behavioral health, long-term services and supports, health-relatedsocial services, and overall member care
- Increasing the member-centeredness and member experience of care
- Adding or improving existing health information technology infrastructure or capabilities, including use of the Mass HIway
- Increasing member access to culturally and linguistically appropriate services and to medical and diagnostic equipment that is accessible to members with disabilities
- Reducing avoidable costs of care, including avoidable inpatient admissions and readmissions
-Increasing the qualityof member care
Investment Strategy to Support Stated Goals: These goals will be achieved with a strong emphasis on care coordination, addressing behavioral health needs, and facilitating a well-integrated system of care with regional and centralized resources to support local care teams. The strategy will be built on a foundation of reliable data so that decisions are informed, and a culture that promotes healthy change to workflows and approaches in order to realize the financial and quality gains we plan to achieve in our new care system. Below is an overview of the strategic DSRIP investment plan:
Anticipated Challenges: Good data has been difficult to obtain. Thus, this program was built on a number of assumptions that may not all hold to be true. As we receive accurate membership, claims, and other types of data, we will adjust our strategy accordingly. In addition, becauseWellforce consists of a number of provider entities, many of which currentlyuse different information systems, an effective integration strategy is paramount. The change in habits and workflows that employees of the organization will have to make to provide truly accountable care may also prove challenging, which has informed Wellforce training programs and program evaluation plans to ensure that care is provided to our patients according to the model we have developed.