Central Processing Unit
The Central Processing Unit (CPU) received 7,630 new referrals for investigation in fiscal year 2018 (FY18) from the following sources:
|
Source |
Number of Referrals |
Percentage of Total* |
|---|---|---|
|
Department of Transitional Assistance |
6,041 |
79.1% |
|
MassHealth |
788 |
10.3% |
|
Hotline |
470 |
6.2% |
|
Data Analytics Unit |
248 |
3.2% |
|
Task Force |
44 |
0.6% |
|
Department of Early Education and Care |
40 |
0.5% |
* Percentages do not total 100 due to rounding.
The following public assistance programs were the primary basis for potential fraud in the 7,630 new referrals:
|
Type |
Number of Cases |
Percentage of Total* |
|---|---|---|
|
Supplemental Nutrition Assistance Program |
3,374 |
44.2% |
|
Transitional Aid to Families with Dependent Children |
1,890 |
24.8% |
|
MassHealth |
1,307 |
17.1% |
|
Emergency Aid to the Elderly, Disabled and Children |
1,010 |
13.2% |
|
Other |
42 |
0.5% |
|
Classification to Be Determined |
7 |
0.1% |
* Percentages do not total 100 due to rounding.
In FY18, CPU processed, analyzed, and reviewed 7,848 referrals. CPU team members identified 2,166 referrals as potential Intentional Program Violation (IPV) cases, where BSI determined that a fraud claim had merit but returned the case to the Department of Transitional Assistance (DTA) for further action based on the evidence, including possible disqualification or recoupment of benefits. Additionally, CPU closed 4,090 referrals administratively with no fraud determined after completing a preliminary investigation. CPU designated 1,592 referrals for case assignment; of those, the MassHealth and DTA Units completed 954 cases.
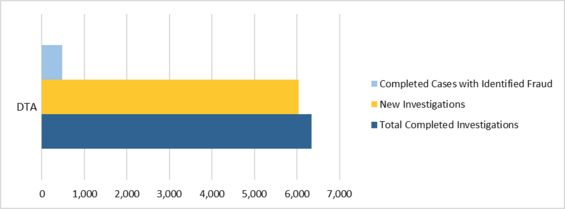
Department of Transitional Assistance Unit
The DTA Unit received a total of 6,041 new cases in FY18, completed 6,340 cases, and identified fraud totaling $4,121,999.16 in 478 cases. The DTA Unit’s breakdown of identified fraud by public benefit program was as follows: $3,025,105.41 for Supplemental Nutrition Assistance Program (SNAP) investigations (21%); $825,564.72 for Transitional Aid to Families with Dependent Children (TAFDC) investigations (6%); and $271,329.03 for Emergency Aid to the Elderly, Disabled and Children (EAEDC) investigations (2%).
In FY18, the DTA Unit filed criminal charges in 13 cases in various courts throughout the Commonwealth. Seven cases resulted in indictments: three in US District Court, one in Suffolk Superior Court, two in Hampden Superior Court, and one in Bristol Superior Court. The remaining six cases were in charged in district courts.
Figure 4. FY18 DTA Caseload
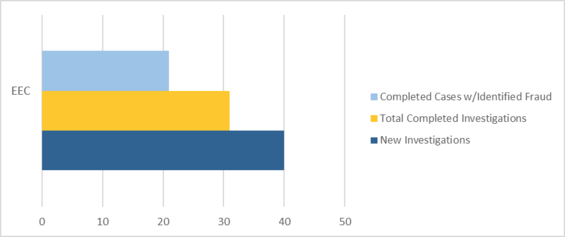
In addition, the DTA Unit received 40 referrals from the Department of Early Education and Care (EEC) and identified $1,548,292.05 in fraud. As part of BSI’s continued working relationship with EEC, EEC’s designated Financial Assistance Worker liaison with BSI is able to efficiently track and assist with BSI’s EEC caseload and provide much-needed documentation and information in an expedited manner for speedier investigations.
Because individuals suspected of defrauding EEC often also receive other forms of public assistance, BSI routinely checks into EEC subjects’ other public assistance benefits and, in particular, their reporting of household income and composition to other agencies. These supplemental investigations have led to the discovery of additional fraud in DTA and MassHealth public benefit programs.
Figure 5. FY18 EEC Caseload
MassHealth Unit
During FY18, the MassHealth Unit received a total of 481 new cases, completed 591 cases, and identified fraud totaling $2,429,372.57 in 324 cases. In addition, the MassHealth Unit contributed to the DTA Unit, including EEC cases, and identified fraud totaling $196,075.23 in 25 cases.
The unit filed four criminal complaints in district courts during FY18. In Lowell District Court, the Massachusetts Attorney General’s Office is prosecuting a defendant for $12,768.00. Another case was filed in Quincy District Court for $48,082.00. A case initially filed in Hingham District Court for $135,014.00 resulted in a grand jury indictment. Finally, in Gardner District Court, a warrant was issued for a defendant charged with fraud in the amount of $18,809.21.
The MassHealth Unit’s continued collaboration with the BSI Data Analytics Unit (DAU) contributed to BSI’s success. The two units successfully investigated personal care attendants (PCAs) who fraudulently received payment from MassHealth by billing the program for services to patients who were in long-term care facilities. MassHealth prohibits PCA services for members who reside in long-term care facilities.
The MassHealth Unit’s relationships with stakeholders within MassHealth—including the Program Integrity Unit, the Executive Office of Elder Affairs, fiscal intermediaries, UMass Medical Center, and the Attorney General’s Office—have led to more frequent meetings, increased communication, and greater efficiency. The unit meets monthly with MassHealth’s management from its Program Integrity and Elder Affairs offices to discuss referrals and their respective workflows. The MassHealth Unit also provides monthly updates on the referrals it has received electronically.
In March 2018, the Assistant Director of the MassHealth Unit and a Senior Fraud Examiner led a presentation for the MassHealth Enrollment Center directors and staff about BSI, the referral process, and BSI’s investigative process. Staff members were encouraged to submit all suspected cases of fraud to the MassHealth Unit and to call with any questions.
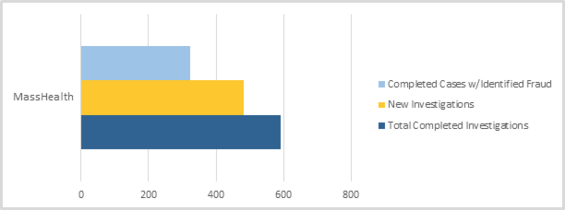
In FY18, the MassHealth Unit conducted 12 civil recoupments, in which subjects entered into repayment agreements with MassHealth totaling $281,505.49. Factors taken into consideration when determining whether to enter into civil recoupment agreements include the subject’s past criminal involvement and the frequency and severity of fraud.
Data Analytics Unit
The growth of BSI’s DAU, its increasing technical capabilities, and its continued collaboration with partners led to 241 referrals: 232 to CPU, and 9 to MassHealth provider-related referrals. The vast majority of the CPU referrals alleged that PCAs falsely submitted timesheets for services to MassHealth members in long-term care facilities. DAU also uncovered PCAs who did not report income earned as PCAs to DTA as required while receiving public assistance benefits.
In addition, using advanced data analysis, DAU was able to identify MassHealth providers, including home health agencies and dental providers, with a high potential for fraud. Ultimately, DAU referred nine cases to outside agencies for prosecution. Seven cases involving MassHealth providers were forwarded to the Massachusetts Attorney General’s Medicaid Fraud Control Unit. The remaining two referrals were forwarded to the federal Office of the Inspector General’s Office of Investigations, which investigates fraud associated with Department of Health and Human Services programs.
DAU continues to support multiple state and federal partners through data assists and joint investigative work, in addition to accepting referrals for investigation and creating and sending referrals to the appropriate entities. For example, DAU is collaborating with federal partners, including the federal Office of the Inspector General’s Office of Investigations on an ongoing investigation that involves multiple home health agencies that have engaged in improper billing practices across both Medicaid and Medicare programs.
| Date published: | March 14, 2019 |
|---|