Central Processing Unit
The Central Processing Unit (CPU) received 3,224 new referrals for investigation in fiscal year 2021 (FY21) and processed, analyzed, and reviewed 3,232 referrals from the following sources.
Table 3. FY21 CPU Referral Sources
|
Source |
Number of Referrals |
Percentage of Total |
|
Department of Transitional Assistance |
1,899 |
59% |
|
Hotline |
571 |
18% |
|
MassHealth |
490 |
15% |
|
Data Analytics Unit |
209 |
6% |
|
Department of Early Education and Care |
31 |
1% |
|
Task Force |
28 |
0.9% |
|
Other |
4 |
0.1% |
The following is a breakdown of the public assistance programs involved in the 3,232 analyzed referrals.
Table 4. FY21 CPU Caseload by Public Assistance Program
|
Type |
Number of Cases |
Percentage of Total* |
|
Supplemental Nutrition Assistance Program |
1,106 |
34% |
|
MassHealth |
901 |
28% |
|
Transitional Aid to Families with Dependent Children |
656 |
20% |
|
Emergency Aid to the Elderly, Disabled and Children |
534 |
17% |
|
Department of Early Education and Care |
31 |
1% |
|
Other |
4 |
0.1% |
* Percentages do not total 100 because of rounding.
CPU team members identified 1,046 referrals as potential intentional program violation (IPV) cases, where BSI determined that a fraud claim had merit but returned the case to the Department of Transitional Assistance (DTA) for further action based on the evidence. Typical agency actions include civil recovery, disqualification, and recalculation of benefits. Additionally, CPU closed 1,533 referrals administratively with no fraud determined after completing preliminary investigations. CPU designated 653 referrals for case assignment. CPU team members continued to carry a small caseload in FY21, completing 54 investigations within the unit.
FY21 was eventful for many reasons. The pandemic continued to impact BSI’s work environment, causing CPU to adapt and, ultimately, improve its internal processes. Despite delays due to challenges faced by external partners working remotely, changes to the benefit programs enacted by Congress, and decreased referrals due to limited personnel, CPU remained committed to providing our investigative staff with comprehensive preliminary case analyses, complete with corroborating documented evidence. During this period, CPU also assisted in the onboarding and mentoring of new BSI team members.
Technology again played a major role in the work of CPU by identifying potential subjects, co-subjects, other identifiers, and addresses; determining the potential breath and width of fraud; and gathering evidence to substantiate fraud. Although team members worked remotely in different locations, CPU seamlessly integrated technology, such as video conferencing and other communication tools, to continue its collaborative team efforts.
CPU team members participated in the vendor selection process, business requirement meetings, testing, and database implementation relative to the new BSI Case Management System (CMS). From inception to going live in June 2021, CPU members were critical to the CMS’s development, testing, and operation.
MassHealth |DTA | EEC Unit
Recognizing that fraud can and often does occur in more than one public benefit program, the MassHealth and DTA units combined to create the Super Fraud Unit. The newly formed Super Fraud Unit consists of seven fraud examiners and three senior fraud examiners who are under the supervision of an assistant director and two supervising fraud examiners.
The Super Fraud Unit completed 629 cases in FY21, which contributed to identifying fraud totaling $4,684,362.51 in 439 cases. The breakdown of identified fraud by public benefit program was as follows:
- $1,891,805.85 for MassHealth (MA) investigations (40.39%)
- $1,890,274.84 for Supplemental Nutrition Assistance Program (SNAP) investigations (40.35%)
- $408,731.78 for Department of Early Education and Care (EEC) investigations (8.73%)
- $338,075.39 for Transitional Aid to Families with Dependent Children (TAFDC) investigations (7.22%)
- $155,271.01 for Emergency Aid to the Elderly, Disabled and Children (EAEDC) investigations (3.31%)
In FY21, due to COVID-19-related court closures and delays, BSI filed criminal charges in just one case in Boston (Boston Municipal Court), which was set for potential settlement by civil recovery following a show cause hearing. Working remotely, coupled with COVID-19 restrictions, halted civil recovery and subject interview efforts at all BSI offices during FY21.
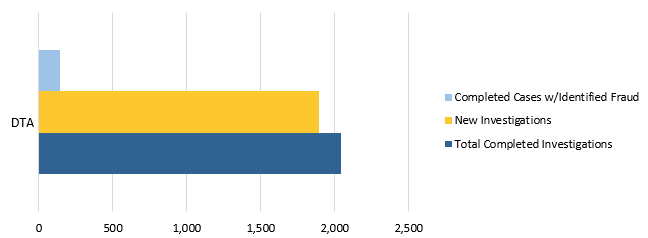
Figure 9. FY21 DTA Caseload
Note: BSI’s DTA caseload for FY21 included SNAP, TAFDC, and EAEDC cases.
Additional changes throughout this fiscal year included BSI and DTA streamlining the method for obtaining electronic benefits transfer history reports. BSI’s CPU unit now collects and submits requests directly to DTA, who generates the requested reports and makes them available to BSI.
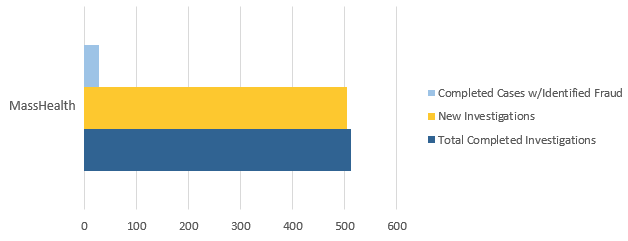
Figure 10. FY21 MassHealth Caseload
BSI’s working relationships with outside stakeholders have always been important, even more so during the last fiscal year. BSI, along with MassHealth and Attorney General’s Office personnel from the Personal Care Attendant (PCA) Task Force, presented to Personal Care Management agencies and Fiscal Intermediaries about PCA fraud investigations. The goal of this presentation was to allow open communication and a better understanding of the work each respective agency conducts.
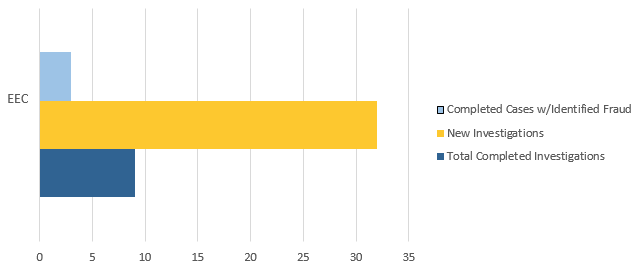
Figure 11. FY21 EEC Caseload
Lastly, the unit completed six investigations that were referred from EEC and identified $297,181.79 in fraud from these referrals. Because individuals suspected of defrauding EEC often also receive other forms of public assistance, BSI routinely checks EEC subjects’ other public assistance benefits and, in particular, their reporting of household income and composition to other agencies. These supplemental investigations have led to the discovery of additional fraud in DTA and MassHealth public benefit programs.
As part of BSI’s expanding working relationship with EEC, EEC permits BSI examiners to participate in EEC’s administrative hearings under the Informal Fair Hearings Rules. The EEC administrative hearing provides BSI examiners the opportunity to explain their investigation and its findings. In FY21, a BSI examiner testified about their investigation at an EEC administrative hearing.
Data Analytics Unit
The growth of BSI’s Data Analytics Unit (DAU), its increasing technical capabilities, and its continued collaboration with partners led to 180 referrals to CPU. The majority of these referrals alleged that personal care attendants (PCAs) failed to accurately disclose their income to the Department of Transitional Assistance (DTA) and MassHealth agencies as required while receiving public assistance benefits. BSI’s DAU also continued to field referrals from BSI’s Public Assistance Fraud Hotline, analyzing seven provider referrals that alleged provider fraud. Many of those investigations remain ongoing.
In addition, using advanced data analysis, BSI’s DAU identified MassHealth providers with a high potential for fraud. The unit identified and referred four MassHealth providers to the Office of the State Auditor’s Medicaid Audit Unit. The unit’s analysis focused on improper billing associated with a variety of dental and physician services. Other analyses conducted by DAU in FY21 focused on services related to vision care, adult foster care, physician services, and the use of certain claim modifiers.
BSI’s DAU continues to support multiple state and federal partners through joint investigative work in addition to accepting referrals for investigation and creating and sending referrals to the appropriate entities. During FY21, BSI’s DAU continued to collaborate with federal partners, including the Office of the Inspector General’s Office of Investigations and the Executive Office of Health and Human Services, on an ongoing investigation related to services provided within both the Medicaid and Medicare programs.
Lastly, BSI’s DAU completed the rollout of its Analytical Support Services, which allows BSI examiners to choose from a suite of services designed to aid in the completion of data analysis tasks associated with their investigations. Services include, but are not limited to, the creation of visualizations (maps, timelines, charts, graphs, etc.) for presentation in court and other settings; the customization of findings reports for the analysis of financial, healthcare, and other relevant data; network and social media analysis; technical training; and Optical Character Recognition services. These services will assist in streamlining and automating several aspects of BSI’s operations.
Other BSI News
During FY21, BSI formed a Training Team to identify staff training needs; build informative trainings, presentations, and job aids; and effectively lead training sessions for all BSI staff. The Training Team was able to successfully create and execute a remote process to conduct civil recoveries and interviews that were previously conducted in-office only. In FY21, BSI initiated repayment agreements and disqualification consent agreements (DCAs) totaling $15,604 following the implementation of the virtual process. DCAs are agreements that subjects sign to disqualify themselves from receiving further DTA and/or EEC benefits because of their IPVs. When pursuing civil recovery for DTA and EEC cases, DCAs are required to complete the civil recovery agreement.
In FY21, the BSI Training Team also hosted mock interview and mock civil recovery trainings, which detailed the processes to conduct each remotely. Examiners actively participated in mock interviews by following partial scripts and watched a video of a mock civil recovery.
During FY21, BSI successfully onboarded four new Fraud Examiners remotely. Using a collaborative team effort, BSI members created a detailed onboarding agenda, which consisted of multiple PowerPoints, job aids, and learning templates. All onboarding materials will serve as lasting guides and remain available on the public drive for all BSI staff members to reference.
FY21 also featured the creation and release of BSI’s new Case Management System (CMS). The new CMS is a platform where all staff members have access to a full case file without physically requesting information from the assigned examiner. The CMS has enhanced the process by which BSI personnel assign cases, request and save documents, request tasks, track case progress, log financials, and generate reports of investigations. The CMS serves as an organized database for examiners to save case files with greater access to management and significantly decreased BSI’s use of and reliance on paper.