Overview
Massachusetts currently has forty open birth hospitals with 986 maternal beds. Signature Healthcare Brockton Hospital is temporarily closed, with 20 maternal beds. Since 2018, four hospitals have closed or filed to close their maternity service (see Figure 1). Additionally, two birth centers have closed, in Beverly and Holyoke. Massachusetts currently has one open free standing birth center: Seven Sisters Midwifery and Community Birth Center in Northampton.
Birth Hospitals and Licensed Beds by EOHHS Region
|
EOHHS Region |
Number of Birth Hospitals |
Maternal Beds |
|---|---|---|
|
Region 1: Western |
6 |
123 |
|
Region 2: Central |
5 |
137 |
|
Region 3: Northeastern |
7 |
161 |
|
Region 4: Metro Boston |
13 |
432 |
|
Region 5: Southeast/Cape |
9 |
133 |
|
MA State-wide |
40 |
986 |
Data source: Facility Master File, July 2023
Massachusetts Performance on Federal Metrics
- MA has no maternity service deserts as defined by March of Dimes1.
- HRSA has defined Maternity Care Health Professional Target Areas (MCTAs) as areas within an existing Primary Care Health Professional Shortage Areas (HPSA) that are experiencing a shortage of maternity health care professionals. MA has four geographic HPSAs which have MCTA scores ranging from 8-12 (of a possible 0-25)2: Gateway Hampshire Regional HPSA (Hampden and Hampshire Counties), Nantucket County, Dukes County, and North Quabbin (Franklin and Worcester Counties.)
| Work Summary | Group Leading | Details |
|---|---|---|
| Levels of Maternal Care | PNQIN with collaborating researchers from DPH | ACOG and the Society for Maternal-Fetal Medicine (SMFM) outlined the Levels of Maternal Care in 2015 as an important strategy to decrease maternal morbidity and mortality. Levels of Maternal Care are framed in assuring that certain resources are available to care for specific maternal conditions and possibly referring women with high-risk comorbid conditions to hospitals equipped with the resources and personnel to manage their unique needs. The ACOG/SMFM guidelines provide a framework for the resources available at a given level of care and example patient comorbidities. These national recommendations left the designation of hospital levels of care and implementation of the paradigm in the hands of the state. The Levels of Care Assessment Tool (LOCATe) was developed by CDC to uniformly assess birthing hospitals’ Level of Maternal Care. The tool, which has been used in half of the states, analyzes hospital survey responses to identify the level of care available at individual hospitals. In 2021, all 40 birthing hospitals in Massachusetts completed the LOCATe survey providing a baseline understanding of current hospital levels of care. The findings are under peer review protection. Note that risk-appropriate care is not synonymous with transferring women to academic medical centers but rather ensuring women have equal access to the services to optimize their birth experience and meet their goals of care. |
| Legislative Report (Chapter 127 of the Acts of 2022, Section 43) | BCHAP | DPH was charged with preparing a report identifying areas where pregnant people do not have access to abortion or birth care within a 50 mile radius. |
| Maternal Morbidity and Mortality Analysis from the Public Health Data Warehouse: Access to and Utilization of Care | OPH, BHCSQ, BFHN, and BCHAP | Examine differences among priority populations in the proportion of women accessing health services: Preventive care (inter-conception/preconception care, Preventive care for WRA is a current Title V priority) and after delivery (hospital readmissions, ED visits and observational stays in the first 6 weeks/year post-birth among women with live births). |
- Nowhere to Go: Maternity Care Deserts Across the US | March of Dimes Maternity
- Maternity Care Target Areas (MCTAs) Scoring | Health Resources & Service Administration (HRSA)
What we can learn from the Kotelchuk index
The Kotelchuck Index, also called the Adequacy of Prenatal Care Utilization (APNCU) Index, uses two crucial elements obtained from birth certificate data: when prenatal care began (initiation) and the number of prenatal visits from when prenatal care began until delivery (received services).
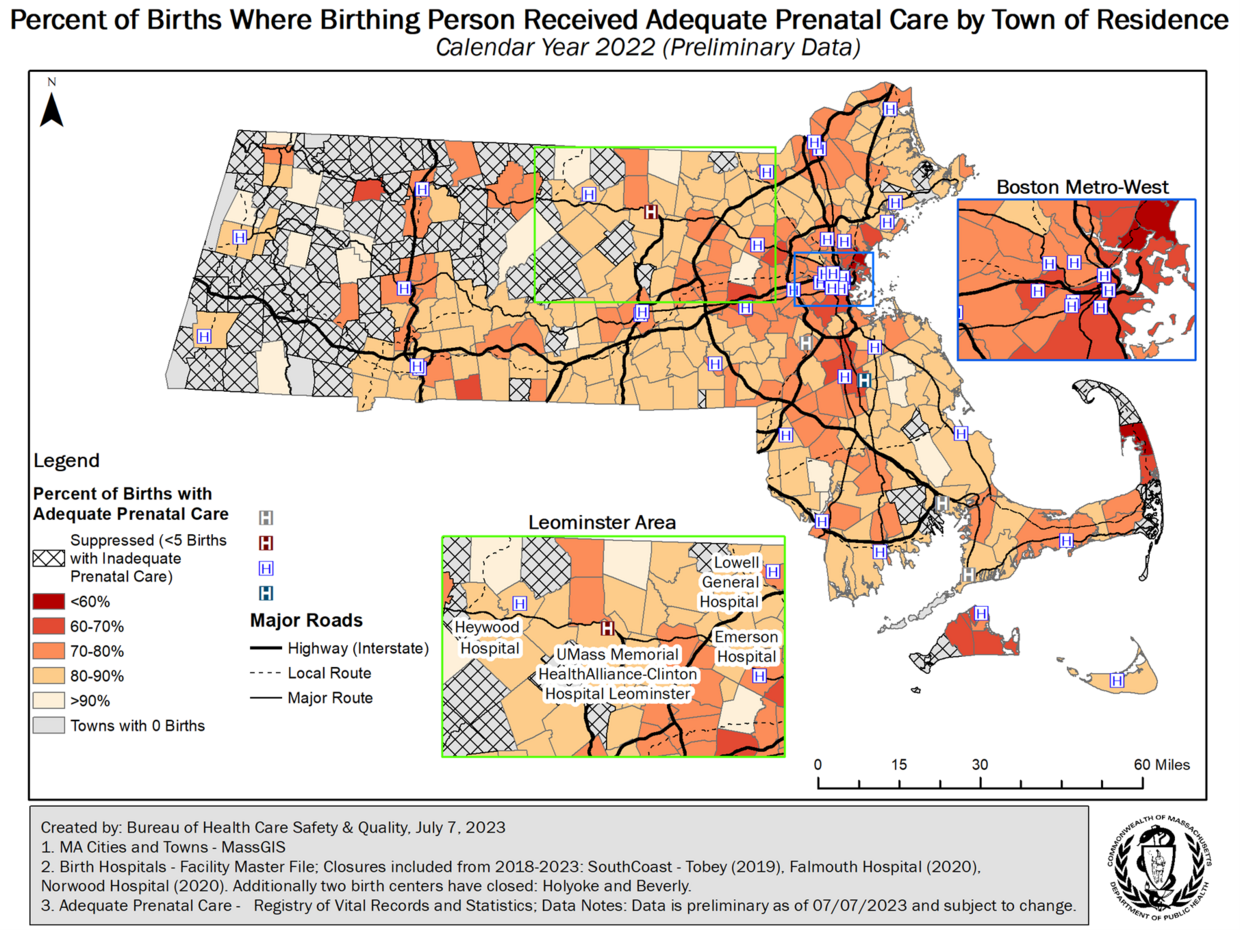
The Kotelchuck Index classifies the adequacy of initiation into four groups, with the underlying assumption that the earlier prenatal care begins the better. To classify the adequacy of received services, the number of prenatal visits is compared to the expected number of visits for the period between when care began and the delivery date. The expected number of visits is based on the ACOG prenatal care standards for uncomplicated pregnancies and is adjusted for the gestational age when care began and for the gestational age at delivery. A ratio of observed to expected visits is calculated and grouped into four categories. The final Kotelchuck Index measure combines these two dimensions into a single summary score. The map below defines adequate prenatal care as a score of 80% or greater on the Kotelchuck Index.
Caveats:
- The Kotelchuck Index does not measure the quality of prenatal care. This is a measure of utilization, people may have access to care but not use it for many reasons.
- Calculation of the Index depends on the accuracy of the patient or health care provider's recall of the timing of the first visit and the number of subsequent visits.
- The Index uses recommendations for low-risk pregnancies, and may not measure the adequacy of care for high-risk women.
Under the text above, please add the figure below:
Figure 1.