Overview
As previously noted, a dual-eligible member’s plan of care describes the types and levels of services that the hospice provider has determined the member needs and that the hospice provider has agreed to provide while the member is in hospice care. Further, under Section 418.24(c) of Title 42 of the Code of Federal Regulations (CFR), effective October 1, 2020, hospice providers are required to develop an addendum to each member’s Medicare Hospice Election Form, titled “Patient Notification of Hospice Non-Covered Items, Services, and Drugs,” that details what services the hospice has determined are not related to the member’s terminal illness and therefore the hospice will not pay for. According to 42 CFR 418.24(c), a hospice must provide this addendum on request to members, non-hospice providers, and/or the Centers for Medicare & Medicaid Services (CMS) within a specific number of days.
For example, the addendum must contain the following:
5. A list of the individual’s conditions present on hospice admission (or upon plan of care update) and the associated items, services, and drugs not covered by the hospice because they have been determined by the hospice to be unrelated to the terminal illness and related conditions.
6. A written clinical explanation, in language the individual (or representative) can understand, as to why the identified conditions, items, services, and drugs are considered unrelated to the individual’s terminal illness and related conditions and not needed for pain or symptom management. This clinical explanation must be accompanied by a general statement that the decision as to whether or not conditions, items, services, and drugs are related is made for each patient and that the individual should share this clinical explanation with other health care providers from which they seek items, services, or drugs unrelated to their terminal illness and related conditions.
Currently, MassHealth does not require hospice providers to submit to it any plans of care. At least three other state Medicaid departments—those of Nebraska, Nevada, and West Virginia—do require hospice providers to submit their plans of care when members first choose to participate in hospice.
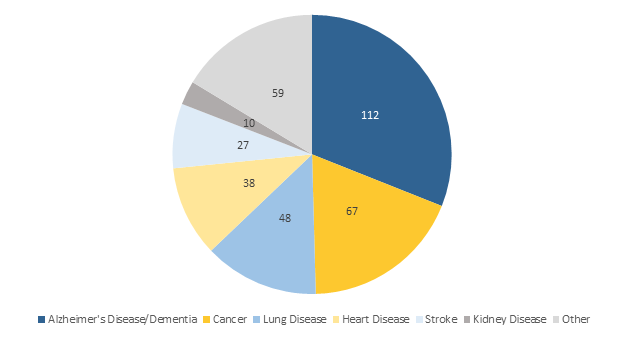
The Office of the State Auditor (OSA) believes that requiring hospice providers to submit plans of care, as well as the information on the addendum required by 42 CFR 418.24(c), would provide MassHealth with information it could use to establish more effective system edits in the Medicaid Management Information System and reduce its risk of improper payments to non-hospice providers. MassHealth could also use this information to monitor services provided to its dual-eligible members who have chosen to receive hospice services to ensure that they receive all the services included in their plans of care. The chart below details the most common types of primary terminal diagnoses for the total 361 members represented in our sample population of 400 claims. The six most common types of primary terminal diagnosis are shown below; they account for 84% of all primary terminal diagnoses in our sample.
In addition, this information would allow MassHealth to ensure regulatory compliance. For example, as previously noted, 42 CFR 418.200 states,
A plan of care must be established and periodically reviewed by the attending physician, the medical director, and the interdisciplinary group of the hospice program. . . . That plan of care must be established before hospice care is provided.
Further, Section 437.422(B) of Title 130 of the Code of Massachusetts Regulations identifies specific requirements for plans of care:
The plan [of care] must include all services necessary for the palliation and management of the terminal illness and related conditions, including the coordination of all in-home supports. The plan of care must be coordinated with any services the member may be authorized to receive from the MassHealth Personal Care Attendant Program and such services may be used only to the extent that the hospice would routinely use the services of a hospice member’s family in implementing the plan of care.
Auditee’s Response
EOHHS will consider this suggestion.
| Date published: | July 20, 2021 |
|---|