Overview
According to the Centers for Disease Control and Prevention (CDC), 1 in 4 adults aged 65 and older falls each year. A fall can result in serious injuries for older adults, including broken bones and hip fractures. About 1 in 4 falls cause a serious injury like a broken bone or head injury, and more than 95% of hip fractures are caused by falling.
Data included in the Special Emphasis Report: Unintentional Fall Injuries among Older Adults, 2006-2014 published by the Injury Surveillance Program and Injury Prevention Control Program, shows that it’s estimated that nursing home residents make up about 18% of elder falls (individuals who are 65 years or older) that result in death.
In Massachusetts, nursing homes licensed by the Department of Public Health (DPH) are required to report when a resident falls and suffers an injury a serious injury to the Bureau of Health Care Safety and Quality. A newly published Special Emphasis Report: Nursing Home Falls with Injury, by Patient Characteristics 2013-2018 uses data reported to DPH to better understand individual characteristics that may increase the likelihood of a fall as well as those that may make it less likely for a resident to suffer a fall.
Nursing Homes Background
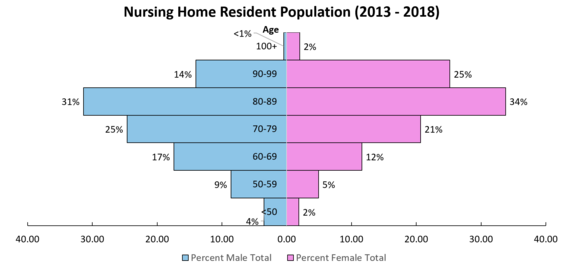
The population of residents living in nursing homes can change regularly, but in a review of residents living in nursing homes between 2013 and 2018, it was found that:
- About two-thirds of nursing home residents were female
- Most nursing home residents were between ages 70 and 99
- 88% of nursing home residents were non-Hispanic white
Risk and Protective Factors for Falls with Injury
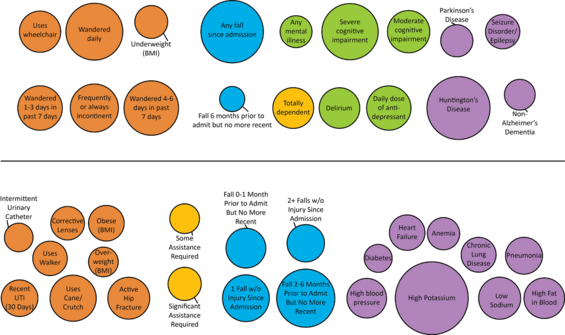
In this graph, if the bubble is above the black line, then that characteristic is considered a risk factor for suffering a fall. A bubble below the line is considered to be a “protective” factor, or a characteristic that may reduce the likelihood of a fall with a serious injury. Each of these factors that were explored were adjusted for age, sex, year of residence in a nursing home, and race.
Findings and Recommendations
Finding: Based on the graph in the previous section, the resident characteristics that have the largest influence in predicting falls with injury included:
- Severe cognitive impairment
- Huntington’s Disease
- If the resident has suffered any falls since being admitted to the nursing home
- Wandering behaviors
Recommendation: Residents with these diagnoses or behaviors should have a robust falls prevention plan that may include alternative activities to engage the residents.
Finding: The resident characteristics that had the largest influence in reducing the likelihood of falls with injury included:
- Advanced disease progression, including high potassium (typically associated with kidney failure), heart failure, and respiratory failure)
- No recent falls, which means that the resident may have suffered a fall up to one month before being admitted to the nursing home or between 2 and 6 months before being admitted to the nursing home, but not more recently than that.
- Uses an assistive device like a cane, crutch, or walker
Recommendation: While being bed bound does decrease the risk for falls, residents with advanced disease progression should be able to participate in activities in the nursing home. Additionally, residents who are able to move around, but may have a history of falls or be at risk for falls, should be encouraged to use assistive devices, as prescribed by the physical therapist, such as a cane, crutch, or walker.
Resources
In Massachusetts, from 2015-2018, 60 nursing homes participated in the Supportive Planning and Operations Team (SPOT) Initiative. Many of the participating facilities used this opportunity to focus on falls prevention work. The quality improvement tools used are available for all nursing homes online.
The Injury Prevention and Control Program makes several falls prevention tips and informational resources publicly available for older adults, caregivers, and health care providers. View Older Adult Falls Prevention resources here.
The CDC has prepared the Stopping Elderly Accidents, Deaths & Injuries (STEADI) toolkit, which may help nursing homes identify best practices for falls prevention. This toolkit and additional resources are available online.
Each September, National Falls Prevention Awareness Day raises awareness about how to prevent fall-related injuries among older adults. Learn more about this falls prevention work on the National Council on Aging’s website here.