Overview
In accordance with Section 12 of Chapter 11 of the Massachusetts General Laws, the Office of the State Auditor (OSA) has conducted a performance audit of certain activities of the Executive Office of Health and Human Services (EOHHS) for the period July 1, 2015 through December 31, 2017.
We conducted this performance audit in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Below is a list of our audit objectives, indicating each question we intended our audit to answer, the conclusion we reached regarding each objective, and where each objective is discussed in the audit findings.
|
Objective |
Conclusion |
|
Yes; see Finding 1, Finding 2, and Other Matters |
|
Audit Constraints
Our audit was initiated to assess whether there were barriers preventing or deterring eligible people from applying for and receiving WIC benefits, as well as how effectively state agencies shared information that would allow them to identify and notify people who might be eligible for WIC benefits but were not receiving them. However, DPH did not provide access to the information we needed to perform our audit work in a timely manner.
Section 7.11 of Chapter 7 of the 2011 edition of the US Government Accountability Office’s Government Auditing Standards states,
Auditors should . . . report any significant constraints imposed on the audit approach by information limitations or scope impairments, including denials or excessive delays of access to certain records or individuals.
During our audit, the following constraints were imposed on the audit process:
- We requested interviews and system demonstrations from the administrators of the six systems operating within EOHHS’s Virtual Gateway (VG) Internet portal during our audit period. However, EOHHS did not comply with this request for approximately one month because of EOHHS management concerns regarding the security of personally identifiable information (PII) maintained in these systems.
- To assess the effectiveness of EOHHS agencies’ data-matching process, we requested that EOHHS provide us with a file that included information on all people who received MassHealth, Supplemental Nutrition Assistance Program (SNAP), Transitional Aid to Families with Dependent Children, or WIC benefits during the audit period. However, this information was never provided. EOHHS instead agreed to generate reports for us that would include SNAP and MassHealth participants who met all eligibility requirements for WIC during the audit period, as well as reports that would identify people who received WIC benefits during that period. EOHHS said we could observe the generation of these reports, but they were not generated until more than two months after we requested them. Moreover, without access to the data that supported these reports, OSA could not assess the data’s accuracy and completeness.
- We intended to interview WIC participants; however, DPH management objected, citing concerns that auditors’ presence would create anxiety for participants that would cause them to drop out of the program. As an alternative to conducting WIC participant interviews, we suggested that we send a survey to solicit comments anonymously. DPH management objected to this approach as well, indicating that it would probably decrease participation in DPH’s own annual WIC participant satisfaction survey, which it planned to distribute soon.
- As an alternative to OSA conducting its own WIC participant satisfaction survey, DPH officials offered to provide us with the responses to DPH’s 2015 and 2016 annual surveys. We did not receive the information until a month later because of DPH management concerns regarding the confidentiality of PII.
Despite these constraints, OSA was ultimately able to perform auditing procedures to meet the audit objectives sufficiently.
To achieve our audit objectives, we gained an understanding of the internal control environment we determined to be relevant to our audit objectives by reviewing the EOHHS Information Systems Internal Control Plan and applicable laws, regulations, and agency policies and procedures, as well as conducting interviews with EOHHS, DPH, DTA, and Office of Medicaid staff members and managers.
Additionally, we performed the following procedures.
Barriers to Accessing WIC Benefits
To determine whether there were barriers preventing eligible people from receiving WIC benefits, we performed the following procedures.
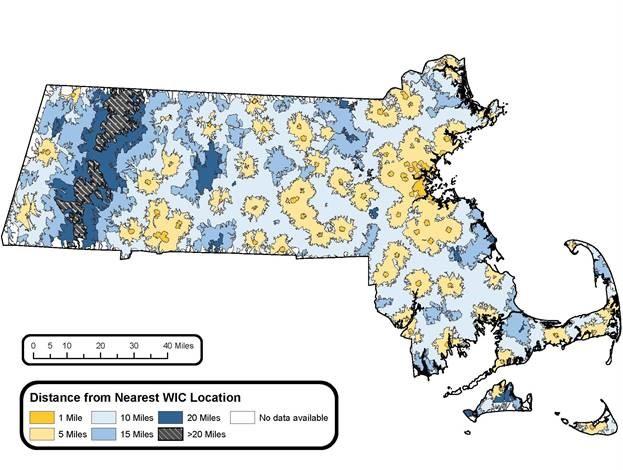
We conducted interviews at a sample of WIC provider locations to gather information related to Eos and to obtain providers’ perspectives regarding barriers that might be inhibiting people’s access to WIC benefits. There are 31 WIC providers that administer 120 locations throughout Massachusetts. The WIC provider locations are indicated below.
Coverage of WIC Providers in Massachusetts
We selected a judgmental sample of 20 locations, representing 16 of the 31 providers and covering all six regions: Boston (6), Cape Cod and the Islands (1), central Massachusetts (3), North Shore (4), South Shore (3), and western Massachusetts (3).
We conducted interviews with DPH personnel and were made aware that the agency performs an annual survey of WIC participants. We received the survey DPH conducted in 2016. We performed completeness and accuracy testing on the electronic spreadsheet containing the survey results before analyzing them.
Data Sharing among DTA, the Office of Medicaid, and DPH
To determine whether DTA and the Office of Medicaid shared data with DPH, we performed the following procedures.
We conducted interviews with EOHHS, DTA, the Office of Medicaid, and DPH to gather information about data sharing that might occur among the agencies. From these interviews, we learned that DPH has data-sharing agreements with both DTA and the Office of Medicaid and that the data are shared quarterly with DPH. We requested, received, and reviewed these agreements. We conducted a follow-up interview with DPH and learned that it shared data in order to identify, and perform outreach to, SNAP and MassHealth consumers who are automatically income-eligible to receive WIC benefits. We observed the quarterly data-matching process at DPH’s offices and received a sample of the postcards that are mailed to the people identified as a result of the data matching. Although DPH was able to demonstrate the data-matching process, DPH does not maintain records of the postcards mailed and therefore could not provide evidence that it had mailed any during the audit period.
We met with DTA’s data analyst to observe the queries he performed to extract data from DTA’s Benefit Eligibility and Control Online Network (BEACON) information system. We reviewed the data properties to verify that the queries extracted the appropriate data for the entirety of the audit period. We also observed the results of the queries that DTA sent to DPH via a secure server.
We met with an Office of Medicaid data analyst to observe the queries he performed to extract data from the state’s Medicaid Management Information System (MMIS). We reviewed the data properties to verify that the queries extracted the appropriate data for the entirety of the audit period. We also ensured the completeness and accuracy of the queries used, and we observed the results of the queries that the Office of Medicaid sent to DPH via a secure server.
We met with DPH to observe its data matching using the data that DTA and the Office of Medicaid had uploaded to DPH’s secure server. We received a file containing the records of unmatched women and children from BEACON and of unmatched women and children from MMIS. DPH’s information technology (IT) specialist proposed an alternative data-matching method that could reduce the number of unmatched records by matching on four specific fields that are likely to be entered consistently in the DPH, DTA, and Office of Medicaid information systems. We accepted her proposal and returned at a later date to receive the results of the data matching using the alternative method.
Data Reliability Assessments
Before observing the process of matching WIC participant data within Eos, we observed the extraction of SNAP participant data from BEACON, and MassHealth participant data from MMIS, to confirm that all data fell within the required date range (July 1, 2015 through December 31, 2017). At DPH’s office, we performed completeness and accuracy testing of the results of DPH’s 2016 annual participant survey to ensure that the data were sufficiently reliable. We also performed a limited review of IT general controls for system access, program changes, and security settings. Based on our audit objectives, we determined that the data from these systems were sufficiently reliable for the purpose of our audit.
Whenever sampling was used, we applied a nonstatistical sampling approach, and as a result, we could not project our results to the entire population.
| Date published: | September 9, 2019 |
|---|