Central Processing Unit
The Central Processing Unit (CPU) received 3,770 new referrals for investigation in fiscal year 2020 (FY20) from the following sources.
Table 3. FY20 CPU Referral Sources
|
Source |
Number of Referrals |
Percentage of Total |
|---|---|---|
|
Department of Transitional Assistance |
2,151 |
57% |
|
MassHealth |
968 |
25.7% |
|
Hotline |
451 |
12% |
|
Data Analytics Unit |
160 |
4.2% |
|
Other |
19 |
0.5% |
|
Task Force |
14 |
0.4% |
|
Department of Early Education and Care |
7 |
0.2% |
The following is a breakdown of the public assistance programs involved in the 3,770 new referrals.
Table 4. FY20 CPU Caseload by Public Assistance Program
* Percentages do not total 100 because of rounding.
|
Type |
Number of Cases |
Percentage of Total* |
|---|---|---|
|
Supplemental Nutrition Assistance Program |
1,661 |
44% |
|
MassHealth |
1,400 |
37.1% |
|
Transitional Aid to Families with Dependent Children |
448 |
11.9% |
|
Emergency Aid to the Elderly, Disabled and Children |
246 |
6.5% |
|
Other |
9 |
0.2% |
|
Classification to Be Determined |
5 |
0.1% |
|
Department of Early Education and Care |
1 |
.03% |
In FY20, CPU processed, analyzed, and reviewed 3,892 referrals. CPU team members identified 778 referrals as potential intentional program violation (IPV) cases, where BSI determined that a fraud claim had merit but returned the case to the Department of Transitional Assistance (DTA) for further action based on the evidence. Typical agency actions include civil recovery, disqualification, and recalculation of benefits. Additionally, CPU closed 2,204 referrals administratively with no fraud determined after completing preliminary investigations. CPU designated 910 referrals for case assignment. CPU team members continued to carry a small caseload in FY20. The unit also completed 51 individual investigations.
In March 2020, with the onset of the COVID-19 pandemic, CPU team members and BSI staff began working remotely. Necessity created the opportunity to think outside of the box and apply technology in order to work efficiently and with minimal interruption while still meeting the unit’s goals and completing vital tasks. The entire agency has become paperless and streamlined; it employs web-based communications using GoToMeetings and Slack. Our video communications simulate the office experience and have improved overall morale, connectivity, and productivity.
MassHealth/DTA Unit
In recognizing that fraud can occur in more than one public benefit program, as shown in BSI investigations, the MassHealth and DTA units combined to create the Super Fraud Unit. As a result, the Super Fraud Unit consists of six fraud examiners and six senior fraud examiners who are under the supervision of an assistant director and two supervising fraud examiners.
The Super Fraud Unit was assigned 573 new cases in FY20, completed 769 cases, and identified fraud totaling $6,172,898.55 in 444 cases. The unit’s breakdown of identified fraud by public benefit program was as follows:
- $2,461.996.60 for MassHealth (MA) investigations (39.9%)
- $2,089,460.76 for Supplemental Nutrition Assistance Program (SNAP) investigations (33.8%)
- $771,178.86 for Transitional Aid to Families with Dependent Children (TAFDC) investigations (12.5%)
- $266,633.86 for Department of Early Education and Care (EEC) investigations (4.3%)
- $165,915.28 for Emergency Aid to the Elderly, Disabled and Children (EAEDC) investigations (2.7%)
In FY20, the unit filed criminal charges in 10 cases in various courts throughout the Commonwealth. Two cases resulted in an indictment in US District Court, while 8 cases were charged in district courts.
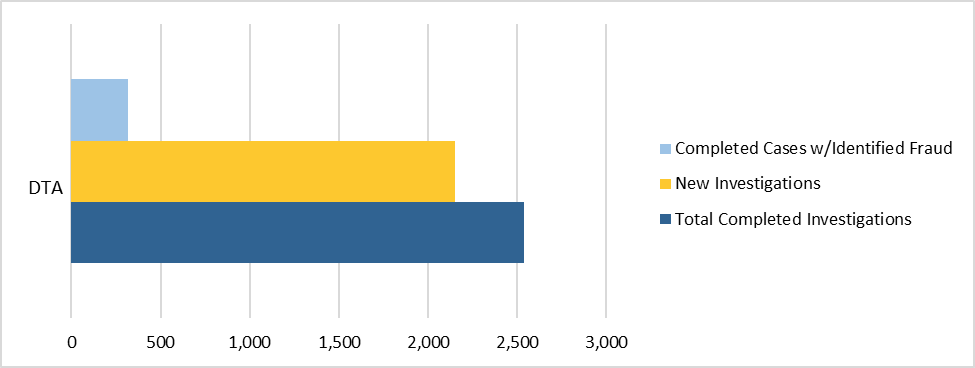
Figure 8. FY20 DTA Caseload
Note: BSI’s DTA caseload for FY20 included SNAP, TAFDC, and EAEDC cases.
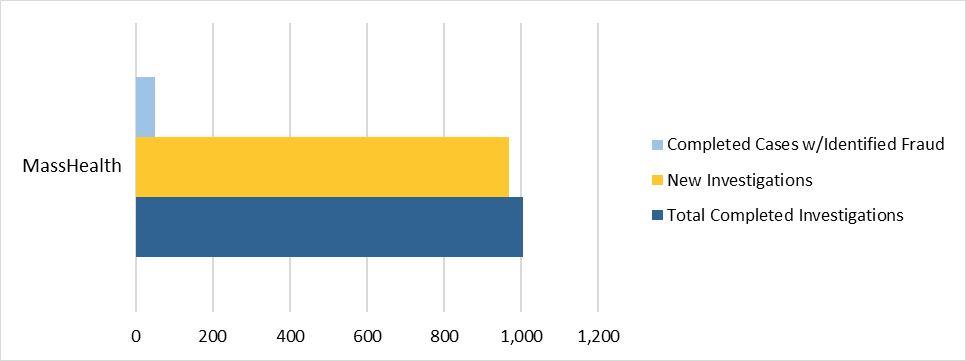
Figure 9. FY20 MassHealth Caseload
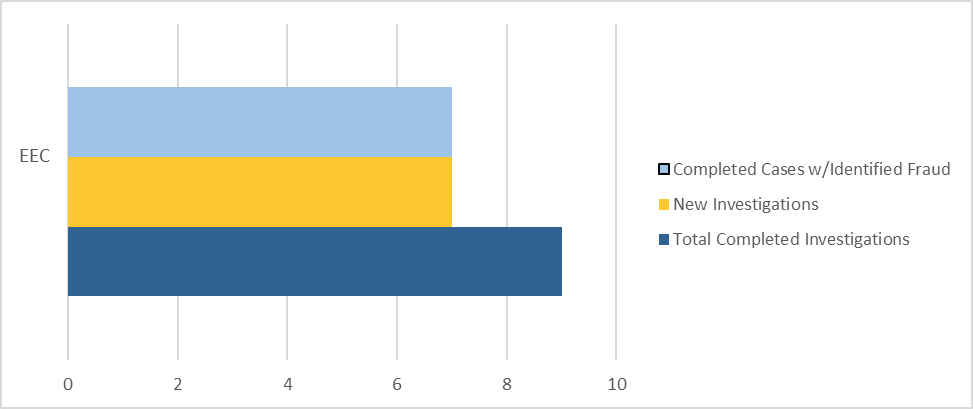
In addition, the unit received seven referrals from EEC and identified $295,288.96 in fraud from these referrals. As part of BSI’s continued working relationship with EEC, EEC’s designated financial assistance worker liaison with BSI is able to efficiently track and assist with BSI’s EEC caseload and provide much-needed documentation and information in an expedited manner for speedier investigations.
Because individuals suspected of defrauding EEC often also receive other forms of public assistance, BSI routinely checks EEC subjects’ other public assistance benefits and, in particular, their reporting of household income and composition to other agencies. These supplemental investigations have led to the discovery of additional fraud in DTA and MassHealth public benefit programs.
Figure 10. FY20 EEC Caseload
The unit also conducted 90 civil recoveries in FY20. In those cases, subjects had the opportunity to enter into repayment agreements with DTA and/or EEC. In FY20, BSI initiated repayment agreements and disqualification consent agreements (DCAs) totaling $2,073,379.24. DCAs are agreements subjects sign to disqualify themselves from receiving further DTA and/or EEC benefits because of their IPVs. When pursuing civil recovery for DTA and EEC cases, BSI requires DCAs rather than administrative hearings.
Data Analytics Unit
The growth of BSI’s Data Analytics Unit (DAU), its increasing technical capabilities, and its continued collaboration with partners led to 1604 referrals to CPU. Indeed, BSI’s DAU’s referrals increased by more than 125% in FY20. The majority of these referrals alleged that personal care attendants (PCAs) falsely submitted timesheets for services to MassHealth members in long-term-care facilities and PCAs were not reporting income earned as PCAs to DTA as required while receiving public assistance benefits. BSI’s DAU also continued to field referrals from BSI’s Public Assistance Fraud Hotline. BSI’s DAU received and analyzed 12 referrals made through the hotline alleging provider fraud, many of which remain ongoing.
In addition, using advanced data analysis, BSI’s DAU was able to identify MassHealth providers with a high potential for fraud. The unit identified and referred seven MassHealth providers. The analysis of these referrals focused on improper billing associated with a variety of healthcare providers and services, including, but not limited to, dental services, hospice services, physician services, evaluation and management services, and the use of certain claim modifiers.
In accordance with the standard operating procedure between Audit Operation’s DAU, BSI’s DAU, and the Office of the State Auditor’s (OSA’s) Medicaid Fraud Unit, BSI’s DAU referred six MassHealth providers to OSA’s Medicaid Audit Unit before FY20. This cross-unit collaboration led to the Medicaid Audit Unit featuring BSI DAU’s findings in four audits issued in FY20. These audits examined adult foster care, home health, and physical therapy services. (https://www.mass.gov/lists/audits-initiated-based-on-referrals-from-bsi)
BSI’s DAU continues to support multiple state and federal partners through joint investigative work in addition to accepting referrals for investigation and creating and sending referrals to the appropriate entities. During FY20, BSI’s DAU continued to collaborate with federal partners, including the Office of the Inspector General’s Office of Investigations and the Executive Office of Health and Human Services, on two ongoing investigations related to services provided within both the Medicaid and Medicare programs.
Lastly, BSI’s DAU continued to collaborate with OSA’s Information Technology team and Audit Operation’s DAU to identify and acquire new software and technology for use by several divisions within OSA. Specifically, BSI’s DAU assisted with the acquisition of OSA’s Optical Character Recognition (OCR) software. BSI’s DAU continues to test this software and will implement the tool in several of BSI’s work processes once complete. The implementation of the OCR software will assist in automating and streamlining several aspects of BSI’s work by electronically converting images into a word, excel, or plain text format and extracting images into searchable files.
| Date published: | February 18, 2021 |
|---|