About the One Big Beautiful Bill Act (OB3)
In July 2025, President Trump signed the One Big Beautiful Bill Act (OB3) into law. This law includes several major changes to Medicaid across the country. MassHealth, Massachusetts’ combined Medicaid and Children’s Health Insurance Program (CHIP) program, is legally required to carry out these changes.
OB3 will require MassHealth to check eligibility for certain members every six months and to require “community engagement,” which includes work, education, or volunteering, for some members. The law will also limit retroactive coverage and eligibility for a limited group of non-citizens.
In addition, the law limits MassHealth’s access to critical federal funds that have been used in the past to support community health centers, hospitals, nursing facilities, academic medical centers, vaccine programs, and more.
How will OB3 impact MassHealth members?
The changes to MassHealth will not happen right away, and they will not affect all MassHealth members.
The first federal change will impact some immigrant members beginning Fall 2026. Other important changes include more frequent renewals and “community engagement.” Under OB3, some members will be required to work, attend educational programs, or volunteer to keep their MassHealth coverage, beginning in January 2027. Starting in 2028, some members, ages 19 through 64, may have to pay for a portion of certain health care services. For more information on these changes and who they will affect, please see the OB3 timeline.
We estimate that hundreds of thousands of people could lose MassHealth coverage because of work requirements, six-month eligibility checks, and other changes. Loss of coverage for these members will not happen all at once. MassHealth is awaiting guidance from the federal government, specifically the Centers for Medicare & Medicaid Services (CMS), to fully understand the policy.
Before any changes happen, MassHealth will contact impacted members and provide information about next steps. These communications will begin in the Summer of 2026.
How can members prepare for these changes?
- Continue to get care, refill prescriptions, and go to your appointments.
- Tell us right away if your contact information changes. It is also important to let us know about changes such as pregnancy, disability status, income, and other factors that could impact coverage. Visit report changes to MassHealth to learn more.
- Read and reply to letters or messages from MassHealth.
- Sign up for MyServices for 24/7 access to your MassHealth.
- Call (800) 841-2900, TDD/TTY: 711, visit a MassHealth Enrollment Center, or find an assister near you if you have questions or need help.
ConnectorCare Plan Type 1
Beginning January 2026, some Massachusetts residents will no longer be eligible for subsidized health care through the Massachusetts Health Connector because of their immigration status. This is due to changes in federal law.
Residents who are no longer eligible for ConnectorCare Plan Type 1 may qualify for MassHealth Limited and the Health Safety Net. MassHealth will send letters to impacted individuals letting them know of their updated eligibility.
For more information about the elimination of Connector Care Plan Type 1, visit the Massachusetts Health Connector.
Learn more about MassHealth Limited and the Health Safety Net.
OB3 Timeline
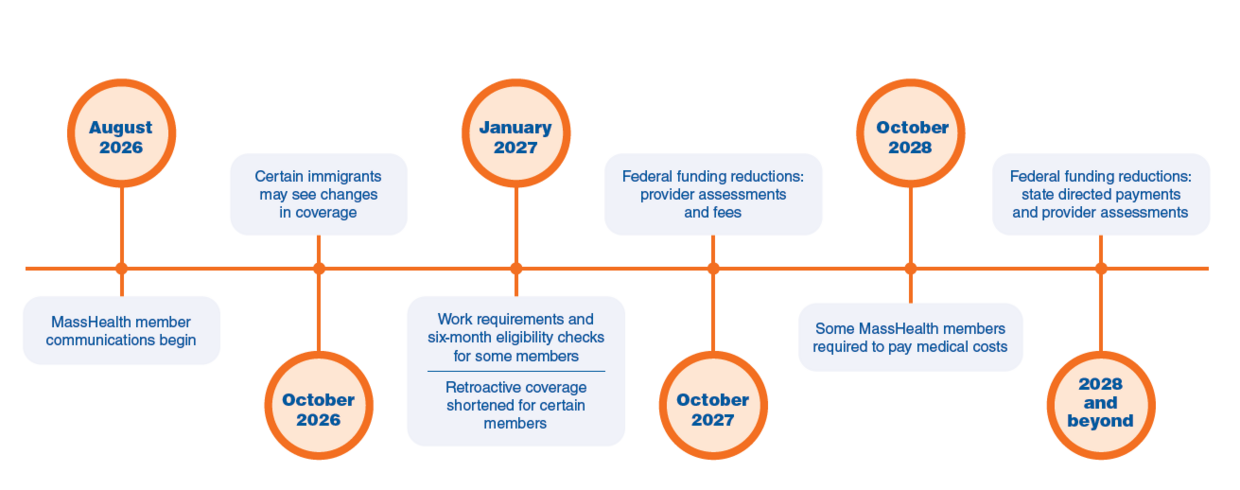
OB3 policies will take effect over the next several years. The high-level timeline below outlines when policies may go into effect. Dates below are subject to change as we receive and work to implement federal guidance and requirements.
August 2026: MassHealth will begin notifying members about changes that may affect them through direct member notices, texts, emails, and more.
October 1, 2026: Some OB3 provisions that affect Alien Medicaid Eligibility for noncitizens take effect. As a result, the federal government will no longer allow certain immigrants who are legally in the U.S. to remain enrolled in Medicaid. This may include refugees, asylees, parolees, and abused spouses.
- We estimate that up to 2,500 members may lose comprehensive MassHealth coverage because of their immigration status.
January 1, 2027: Some MassHealth members will have to comply with work requirements and eligibility checks every six months to receive coverage. In addition, retroactive coverage will be shortened to one month for certain adults, ages 19 through 64, and to two months for other populations.
- Work requirements and six-month eligibility checks will largely impact adults without young children or a disability who are 19 through 64 years old.
- Several populations are exempt from work requirements, including but not limited to:
- Parents or caregivers of
- children 13 or younger or
- an individual with a disability;
- pregnant and postpartum persons;
- individuals who are incarcerated or have been released from incarceration in the past 90 days;
- foster care youth or former foster youth under 26; and
- medically frail individuals.
- Parents or caregivers of
- We estimate that approximately 175,000 people will lose MassHealth coverage because of work requirements and six-month eligibility checks.
- Note: Loss of coverage for these members will not happen all at once. We are awaiting guidance from the federal government, specifically the Centers for Medicare & Medicaid Services (CMS), to fully understand the policy.
October 1, 2027: Federal law will reduce federal funding available through health care related taxes (provider assessments and fees) used to support MassHealth programs and providers.
October 1, 2028: Some MassHealth members will be required to pay a portion of certain medical costs. This population is largely made up of adults, 19 through 64 years old, without children or a disability and with income over 100% of the Federal Poverty Level (FPL).
- For a single adult, this means anyone who earns roughly $16,000 or more will have to pay MassHealth co-payments to receive care. Currently, MassHealth does not require these members to make these payments in order to receive MassHealth coverage or services.
2028 and beyond: Federal law will impose stricter limits on managed care state directed payments and provider assessments. This will reduce federal funding for hospitals and EMS providers.
What is the impact of OB3 on MassHealth’s budget?
MassHealth is jointly funded by the state and federal governments. The federal government reimburses Massachusetts for a portion of MassHealth spending.
There are several changes in OB3 that will reduce the federal government’s contribution to MassHealth spending. These changes include loss of funding due to eligibility changes, October 2027 changes to health care related taxes, and January 2028 changes to state directed payments outlined in the timeline above. This will negatively impact MassHealth members, providers, and the overall Massachusetts health care industry system.
As a result of OB3, Massachusetts estimates that up to 300,000 Massachusetts residents could lose health insurance due to OB3. These reductions in publicly funded coverage, combined with other changes to Medicaid financing, will result in approximately $3.5 billion in federal funding for health care being stripped annually from Massachusetts once the law is fully in effect.
How is MassHealth responding to OB3?
MassHealth’s priority is maintaining coverage and care for as many Massachusetts residents as possible, while complying with these new federal requirements and remaining good stewards of taxpayer dollars. We are committed to working with the legislature, sister agencies, providers, plans, our member advisory council, and other stakeholders to navigate changes imposed by OB3.
While we wait to receive more detailed guidance from the Centers for Medicare & Medicaid Services (CMS), MassHealth is currently:
- Not making any changes for MassHealth members, providers, or plans until we are required to. As we get closer to the start dates for work requirements and more frequent eligibility checks, MassHealth will get in touch directly with impacted members, using notices, robocalls, text messages, or other means of communication.
- Planning to communicate with and train MassHealth staff, community partners, providers, and stakeholder groups who are uniquely positioned to help MassHealth members navigate these new requirements.
Reports of ICE Data Sharing
MassHealth is aware of the report that Immigration and Customs Enforcement (ICE) officials were given access to data on Medicaid members, including home addresses and ethnicities, during the Summer of 2025.
MassHealth uses immigration and citizenship information only as needed to confirm members’ eligibility and to comply with state and federal rules. MassHealth is legally required to share member information with the federal government, specifically the Centers for Medicare & Medicaid Services (CMS).
We object to this sharing and maintain that it violates federal law. Massachusetts has joined a lawsuit over CMS’ sharing of Medicaid data with ICE.
For a list of immigration services in the community, visit Immigrant Health Toolkit – Health Care For All.
| Date published: | November 26, 2025 |
|---|