Overview
MassHealth develops sub-capitation per-member, per-month (PMPM) rates that are unique to each group of practices that corresponded to a single tax identification number (TIN) and are enrolled in a MassHealth Accountable Care Organization (ACO). Sub-capitation PMPM rates for each TIN are based on historical fee-for-service claims for a defined set of primary care services. Sub-capitation PMPM rates are set annually and remain consistent throughout the year. This methodology will be subject to change as MassHealth moves toward population-based rates rather than TIN-specific rates.
Rate Development Objectives and Approach
1. Historical Base Rates: Define primary care costs by using a set of historical claims for MassHealth members, and MassHealth primary care claim logic
To maintain stable primary care revenues, MassHealth estimates the historical per month costs of primary care services for each TIN. This calculation is done in three steps. As a first step in rate development, MassHealth ACOs identify the TINs that have primary care panels and the MassHealth members attributed to each TIN. MassHealth only includes claims billed for the TIN’s attributed members in the historical base period. Second, MassHealth further narrows claims to only those that have CPT codes included in the current primary care sub-capitation service code set. Last, MassHealth only includes claims rendered by providers with a qualifying provider type and specialty. This third step does not apply for community health centers (CHCs). At CHCs, all claims for primary care-related service codes are included, irrespective of the provider specialty.
To account for the different care needs and costs of different member populations, MassHealth separates each TIN’s historical base claims into four categories that vary by the age and disability status of the attributed members who receive care: adults with disabilities, adults without disabilities, children with disabilities, and children without disabilities. This is the historical primary care sub-capitation dollars varied by each population category.
To calculate the PMPM, MassHealth divides the historical primary care sub-capitation dollars for each population category by the number of members attributed to the TIN within each population category over the same period. The overall sub-capitation historical base rate for each TIN is a weighted average of these population-specific PMPMs.
2. Prospective Actuarial Adjustments: Adjust rates to reflect future changes in primary care costs and utilization
After determining the historical base rate, MassHealth and its actuaries apply adjustments to estimate how future primary care costs would differ from historical ones. These adjustments are based on expected market changes and follow standard actuarial principles. The adjustments seek to: 1) set unit costs of claims to the standard, most recently available MassHealth fee schedule; 2) account for year over year growth in medical expenditures (both unit costs and utilization); 3) account for any changes to the program, services, or unit costs that occurred after the historical period; 4) minimize revenue volatility for a subset of TINs that have a low number of claims or attributed members over the historical period. These adjustments vary by category of service, provider type, and population category, but they do not vary by individual member or TIN.
3. Clinical Tier Enhanced Payments: Incentivize care delivery transformation
To grow investment in primary care and incentivize practices to transform care delivery capabilities, MassHealth added a clinical tier enhanced payment to the rates described above. Each practice site attests to a clinical tier (1, 2, or 3) based on meeting a set of clinical criteria. Clinical tier enhanced payments vary by tier and by member age, as indicated in the table below. To account for the fact that a TIN may include multiple practice sites at different tiers, overall, TIN-level PMPM rates include a weighted average of the clinical tier enhanced payments among practice sites associated with each TIN. For more details, see the section Care Delivery Transformation.
2024 Clinical Tier Enhanced Payments (component of PMPM rate) | Pediatric Members | Adult Members |
|---|---|---|
| Tier 1 | $5.20 | $4.16 |
| Tier 2 | $7.28 | $6.24 |
| Tier 3 | $13.52 | $10.40 |
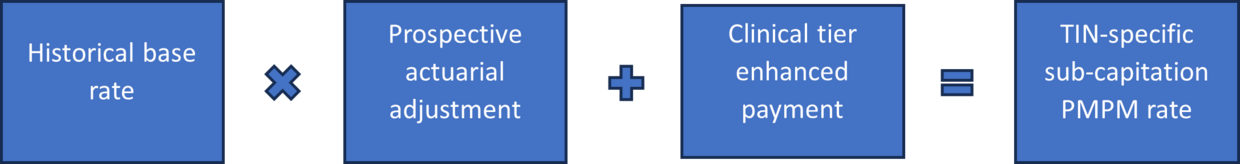
Putting It All Together
In the first years of Primary Care Sub-Capitation, ACOs made sub-capitation payments to TINs based on the members attributed to practices associated with the TIN. Sub-capitation PMPM rates were set at the TIN level. Sub-capitation rates were based on a historical base of claims for a set of services included in the Primary Care Sub-Capitation Program, as defined by the MassHealth claim logic. The historical base was calculated separately for different member populations (e.g., adults without disabilities, adults with disabilities, children without disabilities, children with disabilities), and each TIN’s overall historical base rate was calculated as a weighted average across these populations. MassHealth and its actuaries applied prospective rate adjustments to account for the ways in which future primary care costs would differ from historical ones. The final TIN-specific sub-capitation PMPM rates included a clinical tier enhanced payment based on the weighted average of the clinical tiers of practice sites associated with that TIN.