What is MOLST?
Healthcare providers should continue using the MOLST form until further notice.
MOLST is not for everyone. It is intended for people with serious illness to document their treatment choices in the event of a medical emergency. MOLST is voluntary and should be completed by a medical provider after discussion with the patient.
MOLST is a medical order form (similar to a prescription) that relays instructions between health professionals about a patient's care. MOLST is based on an individual's right to accept or refuse medical treatment, including treatments that might extend life.
MOLST is very different from a health care proxy form. All adults aged 18 and older should complete a health care proxy form to name the person who can make medical decisions for them in the event of an unexpected illness or accident. Whenever possible, the Health Care Agent should be included in conversations about MOLST.
Completion of a MOLST requires discussions between the signing clinician (physician, nurse practitioner or physician assistant), the patient, and family members/trusted advisors about:
- The patient's current medical condition
- What could happen next
- The patient's values and goals for care and
- Possible risks and benefits of treatments that may be offered
After these discussions, the MOLST form is filled out and signed by the clinician to instruct other health professionals about the use of life-sustaining treatments for the patient, based on the patient's own expressed wishes. The patient signs the MOLST form.
The signed MOLST form stays with the patient and is to be honored by health professionals in any clinical care situation. Learn more about MOLST by clicking on the links below:
For Providers
For Consumers
For questions about MOLST, email: MassachusettsPOLST@mass.gov
For information about Health Care Proxy, go to Quick Start - Honoring Choices Massachusetts
About the MOLST to POLST Transition
Massachusetts is transitioning from the MOLST form to the National POLST model.
The MOLST form is still valid and should be used to document patients’ wishes until further notice.
Previous POLST test sites should continue to use the POLST in paper format, and should be considered valid by EMS and other healthcare professionals.
What is POLST?
POLST is a PROCESS in which:
- Patients are identified by their medical providers as having a serious illness or advancing frailty.
- Conversations take place between a patient and their provider about their medical condition, treatment options and what matters most to them.
- A medical order is completed that reflects the patient’s treatment choices. The form is valid regardless of where the patient is receiving treatment (portable).
- For more information about POLST, visit About - POLST
Why is Massachusetts transitioning from MOLST to POLST?
Under the Executive Office of Aging & Independence (AGE), in partnership with the Department of Public Health and the Executive Office of Health and Human Services, MassPOLST is responsible for the state-wide transition to the National POLST paradigm. This includes the design, development, and implementation of an electronic registry (ePOLST Registry), provider training, and consumer education, among other things. See enabling legislation for more detail.
When will Massachusetts transition to POLST?
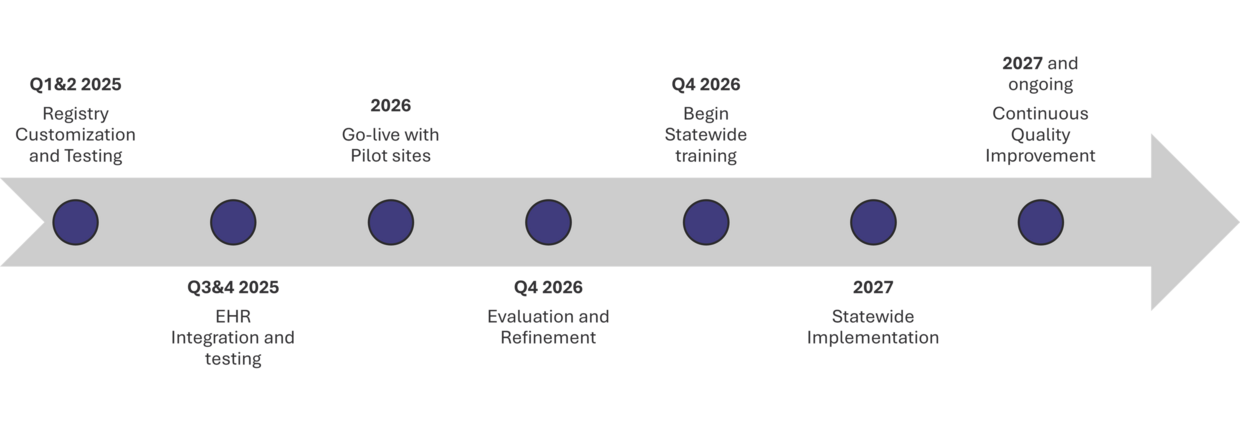
We anticipate state-wide rollout to begin 2027. Here is the estimated Implementation Timeline:
What can healthcare organizations do to prepare?
- Identify Transition team – be sure you have the right people at the table (IT, Clinical, PM, QI)
- Engage executive leadership – what is needed for prioritization and implementation from organization perspective
- Signup Form to receive updates and invitations to statewide meetings