Rates
The sub-capitation per-member, per month (PMPM) rate covers the average monthly per-member costs for a defined set of primary care services, and it is developed based on a historical period of fee-for-service (FFS) claims for these services. Any services that are not part of the primary care sub-capitation set of services are paid FFS. Please refer to the section Rate Methodology for more details.
As part of the overall PMPM rate, practices receive a “clinical tier enhanced payment” each month that accounts for and incentivizes investments in enhanced primary care capabilities. Practices fall into one of three clinical tiers based on a set of criteria. Enhanced payments increase by clinical tier to reflect more advanced capacity to provide integrated, team-based care. For more details, please refer to the section Care Delivery Transformation.
Claims Processing
Under Primary Care Sub-Capitation, practices must submit claims for all services provided. For services that are not covered by the sub-capitation PMPM rate, providers are paid FFS. For services that are covered by sub-capitation, claims are “zero-paid” because these services are reimbursed through the sub-capitation PMPM rate. To determine if a claim is included in the primary care sub-capitation PMPM, and therefore, should be zero-paid; MassHealth considers the following:
- Does the patient meet the Member Attribution criteria?
- Is the CPT code included in the current code set?
- Were the services rendered by a provider with a qualifying provider type and specialty?
For example, a claim submitted by a group practice organization with CPT code 99213 for a patient visiting their pediatrician would be zero-paid as this service is included in the sub-capitation PMPM. If the member attribution, CPT code, provider type, or provider specialty on the claim indicate that the services provided were not covered under the sub-capitation PMPM, the claim would be paid FFS.
Flow of Funds
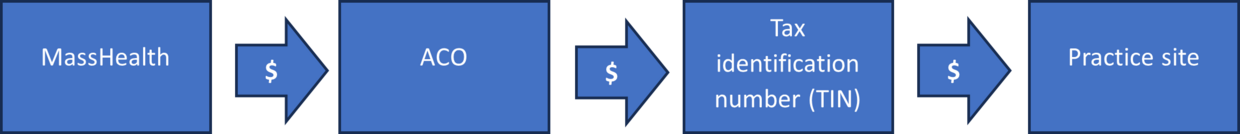
MassHealth pays its Accountable Care Organizations (ACOs) a monthly capitation for each member enrolled. A portion of this is allocated to the Primary Care Sub-Capitation Program (this is why it’s called a “sub-capitation” – it’s a capitation that falls within the broader capitation payment to the ACO).
MassHealth develops primary care sub-capitation rates at the tax identification number (TIN) level. A TIN could correspond to a single practitioner, single practice’s office site, several sites, or in some cases, a large multispecialty group of providers. ACOs are contractually obligated to make sub-capitation payments to each participating TIN for all members attributed to that TIN each month (Accountable Care Partnership Plan Contract Section 2.23.A.1.h, Primary Care Accountable Care Organization Contract Section 2.14.A.1.h). If there are multiple unique practices that share one TIN, the ACO or TIN may determine how the base rate is allocated to each practice, as long as each practice’s clinical tier is reflected in their payment. TINs will receive the PMPM payment each month; however, ACOs must adjust payments regularly to accurately reflect changes to MassHealth enrollment or to the practice’s patient panel. MassHealth monitors and enforces payment requirements on a regular basis.
| Date published: | July 1, 2024 |
|---|