About the Data
The chronic disease hospitalizations dataset includes information on stroke, mental health, diabetes, cardiovascular disease, and cancer.
The data set includes age-adjusted and crude hospitalization and emergency department visit rates per 100,000 people in a given geographic area for Massachusetts and non-Massachusetts residents.
As you look at data on this webpage, you may see differences among population groups. The differences are especially noticeable between white people and people of color.
These differences exist because of structural racism. These differences are NOT because of an individual’s choices, behaviors, or identity.
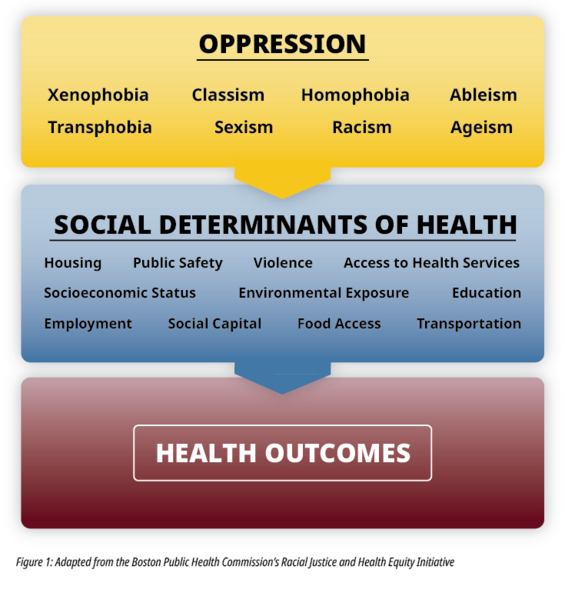
Systems of oppression, such as racism, cause harm to everyone. They also influence the social determinants of health (SDoH), which impact health outcomes. See Figure 1.
It is important to keep these notes in mind when looking at the data and using it to inform public health efforts.
If you decide to share these data, remember to use racial equity context and framing. The DPH Racial Equity Data Road Map is one resource that can help.
About Chronic Disease Hospitalizations
Chronic disease hospitalizations data are presented as two measures on this site: Hospital Admissions and Emergency Department (ED) visits. The hospital admissions measure includes patients who are admitted to the hospital, treated as inpatients, or were admitted for observation. The ED visits measure includes patients who are treated and released in the ED.
Chronic disease data can be used to monitor trends over time, identify communities and populations at increased risk for adverse outcomes and mortality, guide chronic disease management and prevention programs and policies, and evaluate chronic disease management and prevention strategies.
Stroke
A stroke occurs when the normal blood flow to the brain is disrupted, either by a clot or a ruptured blood vessel. Without oxygen provided by the blood flow, the brain cells begin to die. Quick identification of stroke when it occurs as well as timely treatment can prevent disability and death. A key measure to prevent stroke is controlling blood pressure in persons who have hypertension-a condition where a person’s blood pressure is too high.
In Massachusetts, there are over 16,000 hospitalizations due to stroke in a given year, with the highest burden experienced by people of color. The rate of stroke hospitalizations for non-Hispanic, black residents is 74% higher than that of non-Hispanic, white residents, inequities that are driven by structural and interpersonal racism as well as inequitable access to preventative care. Stroke also demonstrates marked inequities by income: according to the 2012 Behavioral Risk Factor Surveillance System, 6.9% of Massachusetts adult residents with less than $25,000 per year in household income reported ever having had a stroke, compared to 1.6% of Massachusetts adult residents with greater than $75,000 per year in household income. These outcomes are driven by inequitable access to preventative care.
Mental Health
Generally, mental health refers to a person’s psychological, emotional, and social wellbeing. Mental health challenges such as depression, anxiety, schizophrenia, and suicidality, are common. Mental health is impacted by myriad factors, including social support, community and cultural connectedness, traumatic experiences, family history, access to treatment, and financial health, to name a few. With treatment and support, people experiencing mental health challenges can recover and live a full, healthy life.
According to the 2016 Behavioral Risk Factor Surveillance System, 11.3% of Massachusetts adult residents reported having 15 or more days of poor mental health. Massachusetts adult residents with less than $25,000 per year in household income have markedly higher prevalence of poor mental health compared to Massachusetts adult residents with greater than $75,000 per year in household income: 21.3% compared to 7.2%, respectively.
Diabetes
Diabetes is when a person’s blood sugar (also called blood glucose) is too high. Normally, the body produces a hormone called insulin that turns blood sugar into energy and keeps blood sugar within a healthy range. When a person has diabetes, their body either does not produce enough insulin or cannot use insulin correctly.
When diabetes is not controlled, it can lead to serious health issues, such as organ damage and blindness. Using data from the 2016 Behavioral Risk Factor Surveillance System, it is estimated that 9.3% of Massachusetts adult residents reported having diabetes. Mortality associated with diabetes demonstrates considerable racial inequities: non-Hispanic, black residents experience over the twice the rate of mortality due to diabetes compared to non-Hispanic, white residents. These inequities are a result of racism, both structural and interpersonal, and inequitable access to healthy environments.
Cardiovascular Disease
Cardiovascular disease is a broad term that includes many different conditions of the heart and blood vessels. The most common kind of cardiovascular disease is coronary artery disease, where the blood vessels that provide oxygen to the heart harden and narrow. This can lead to a heart attack or stroke.
Cardiovascular disease was the second leading cause of death in Massachusetts in 2014. In 2016, 5.5% of Massachusetts adult residents reported having been diagnosed with coronary artery disease or angina (severe pain in the chest due to lack of blood flow to the heart), estimated from the statewide Behavioral Risk Factor Surveillance System. Household income, a major determinant of access to preventative care and resources to prevent chronic disease, demonstrates marked inequities-Massachusetts adult residents with less than $25,000 per year in household income are over 3 times more likely to report having been diagnosed with coronary artery disease or angina compared to Massachusetts adult residents with greater than $75,000 per year in household income.
Cancer
Cancer is a broad term that includes many diseases. Cancer occurs when the body’s production of new cells is too active. Normal adult cells only divide to repair or replace damaged cells, but cancers cells cannot stop dividing and spread. Cancers are named after the part of the body where it starts, for example breast cancer or skin cancer.
Cancer was the leading cause of death in Massachusetts in 2015. Unfortunately, it is not possible to predict who will get cancer and who will not. In addition to its morbidity and mortality burden, cancer has high economic costs. In 2015 the Agency for Healthcare Research and Quality (AHRQ) estimated that the total direct medical cost of cancer in the US was $80.2 billion. In Massachusetts, the total cancer cost cancer in 2010 was $3.318 billion and is projected to be $6.17 billion by 2020.